Apr 4, 2019
A patient presents to the office because of pain in the knee with or without a history of injury. An examination is performed followed by an X-Ray. Osteoarthritis may or may not be seen on the X-ray. If there is an altered range of knee motion when compared to the “normal” side, then a preexisting condition is considered. Whether or not the physician considers arthritis, an MRI is requested. The MRI report 48 hours after imaging is consistent with a torn medial meniscus. Should all patients with a torn medial meniscus undergo surgical intervention? If surgery is undertaken, should the procedure be a repair or a partial removal? The management of meniscal injuries must be influenced by the knowledge that meniscal integrity is important in load distribution across the joint. Meniscal injury causes altered joint mechanics and is related to the onset of arthritis.
According to a recently published online article in the British Journal of Sports Medicine, arthroscopic partial meniscectomy (APM) may not be the best option for all patients with knee pain and meniscal tear. Researchers investigated patients with meniscal tears that compared Arthroscopic Partial Meniscectomy to nonsurgical intervention, pharmacological intervention, and no intervention. At six to 12 months, APM patients had a slight improvement in knee pain, knee-specific quality of life, and knee function compared to physiotherapy patients. When excluding osteoarthritis (OA) patients, the aforementioned outcomes exhibited small to moderate improvement. Knee pain, function, and quality of life did not improve for APM patients compared to placebo surgery patients at six to 12 months regardless of OA status.
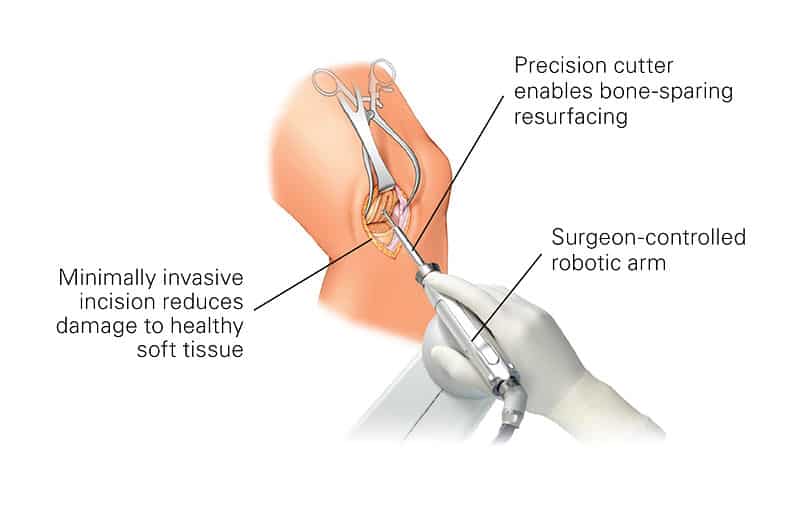
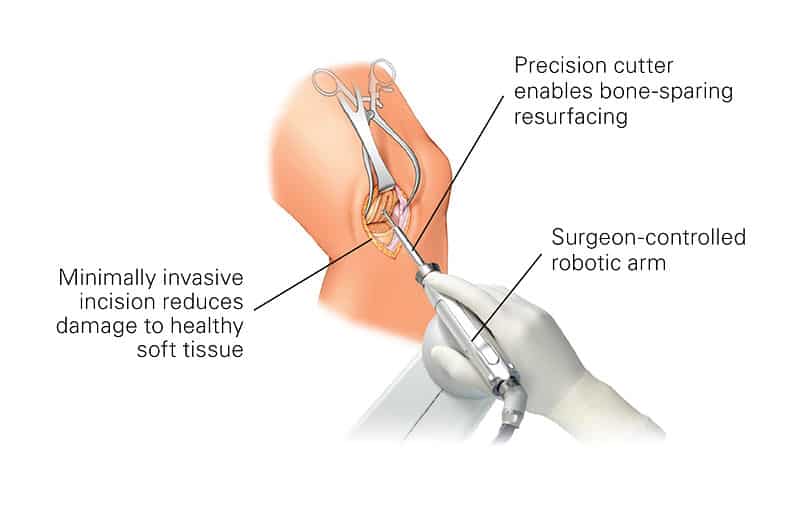
There may, however, be a small-to-moderate benefit from APM compared with physiotherapy for patients without osteoarthritis and who have mechanical or obstructive signs. Arthroscopic partial meniscectomy (APM), a keyhole surgery where loose and fragmented pieces of a torn meniscus is removed, is one of the most common orthopedic procedures performed. Over half of these are performed to treat a meniscus tear in a degenerative knee; however, several recent randomized trials have shown that Arthroscopic Partial Meniscectomy is not superior to conservative treatment or placebo treating meniscus tears associated with a degenerative knee. On the other hand, there is universal agreement that the traumatic meniscus tear, the result of a knee injury in a younger patient with otherwise healthy knee (with no degeneration), should be treated by surgery.
Then what is the downside of meniscal injury and surgery? The medial and lateral meniscus together provide shock absorption, establish a broad base of contact surface and help provide stability to the knee. Those who have undergone total or partial meniscectomy should understand that in five to 15 years, they will develop degenerative arthritis. The long-term outcomes of those whose tears were treated by repair rather than removal has not been established. My Regenerative Medicine practice in part, is the result of those seeking to postpone or avoid a Total Knee Replacement years after a meniscal injury followed by arthroscopic surgery. As long as the arthritis has not progressed to a Grade 4, I am able to assist the patient with joint restoration, at times joint regeneration, it is matter of age and health. While I am able to offer joint restoration, on occasion, joint restoration for those who sustained meniscal and Anterior Cruciate injury in the past, is there anything that could be used as an adjunct at the time of the meniscal injury to promote healing without surgery or postpone, perhaps avoid future postraumatic arthritis?
To learn more. Schedule a consultation (312) 475-1893.You may view my web site at www.sheinkopmd.com.
Tags: ACL, ACL Injury, anterior cruciate, arthritic knee, arthritis, Autologous Protein Concentrate, baseball, BMC, board-certified, Bone Marrow Concentrate, bone marrow edema, cells, cellular orthopedic, cellular orthopedics, FDA, football, golf, Growth Factors, hematopoietic cell, injection, Interleukin 1 Receptor Antagonist Protein, IRAP, joint health, joint pain, knee replacement, lipogems, meniscal injury, meniscectomy, Mesenchymal Stem Cell, micro-fragmented adipose, muscle injury, muscle strain, OA, Orthopedic Surgeon, Osteoarthritis, pain, Physical Therapy, Platelet Rich Plasma, platelets, PRP, regenerative medicine, repair, Rotator cuff tear, soccer, sports injuries, sports medicine, stem cells, strain, tear, torn medial meniscus, training, volleyball

Mar 28, 2019
Opening day of the baseball season is today, Thursday, March 28. I noted this morning on the sports pages how many players will not be available for the start of the race owing to injuries sustained in Spring training. In the basketball coverage, from the get go of March Madness to now, most teams have been playing at times without a star owing to injury. Then there are the final weeks of hockey, will Chicago make the playoffs? Certainly, injury could play a major role. Next in line are the joggers, cyclists, tennis players, so on and so forth who will soon be unable to meet their recreational goals owing to tendon, muscle and ligament injury. With spring comes strains and sprains.
The term strain applies to the over stretching or tearing of muscles and tendons; while a sprain is the overstretching or tearing of a ligament. The most common location for a muscle strain is the hamstring; while the most common location for a sprain is at the ankle joint. Stretching muscle and tendon groups is the best prevention for strain. At this time of the year, especially for the weekend warriors, stretching strengthening and hydration are paramount for minimizing injury.
In spite of the best of fitness preparation and compliance, you feel that stabbing pain in your calf, in the back of the thigh, in your low back in the area of the shoulder. You may choose to take advantage of direct access to the physical therapist. Should you have a greater concern regarding the nature and severity of an injury, call for an orthopedic assessment. After a physical examination, the X-ray, Ultrasound or MRI may be ordered for a most accurate diagnosis or to grade the severity of injury. If and when, physical therapy, anti-inflammatories, or a cortisone injection do not provide relatively short-term relief, it may be time to consider a regenerative medicine intervention. For sports injuries, Platelet Rich Plasma is increasingly proving effective in promoting healing, minimizing impairment, and allowing for the quickest return to highest levels of performance. The major determinant of success is the quality of the PRP as measured by either ratios of protein, platelet and cellular content; or by the actual platelet content of the plasma itself.
While in some clinics, Platelet Rich Plasma is produced by a blood draw and centrifuging, there is no standardization or quality control. In my practice, we create a known and standardized PRP. At the beginning, a finger stick is leads to a platelet count of the patient’s circulating blood. Next, the number is entered into a computer algorithm taking into account the proprietary kit being used as well as the ultimate platelet concentration and plasma volume following the centrifuging process. A repeat platelet count is done prior to injection making sure that desired numbers have been reached. if not, we are able to adjust numbers and concentration to the sought-after target. In this way we can customize the platelet Rich Plasma for each patient’s needs. Once prepared, an ultrasound unit is employed to assist targeting and making sure the PRP is injected into the desired location; that is the site of injury. The procedure is standardized in our office but customized for the shoulder, elbow, hamstring or calf. On occasion, the process may have to be repeated in three to six weeks for maximum benefit. Don’t let an injury ruin your season; if usual and customary is not effective, call for an appointment.
For more information, visit https://sheinkopmd.com or call (312) 475-1893 to schedule a consultation.
Tags: ACL, ACL Injury, anterior cruciate, arthritic knee, arthritis, Autologous Protein Concentrate, baseball, BMC, board-certified, Bone Marrow Concentrate, bone marrow edema, cells, cellular orthopedic, cellular orthopedics, FDA, football, golf, Growth Factors, hematopoietic cell, injection, Interleukin 1 Receptor Antagonist Protein, IRAP, joint health, joint pain, lipogems, Mesenchymal Stem Cell, micro-fragmented adipose, muscle injury, muscle strain, OA, Orthopedic Surgeon, Osteoarthritis, pain, Physical Therapy, Platelet Rich Plasma, platelets, PRP, regenerative medicine, repair, Rotator cuff tear, soccer, sports injuries, sports medicine, stem cells, strain, suntimes, tear, training, volleyball

Mar 22, 2019
I will let the scientific facts speak for themselves. Keep this in mind the next time you see the advertisement from the Stem Cell hustlers of America. There is no such thing as a free lunch.
From: The American Journal of Sports Medicine
Are Amniotic Fluid Products Stem Cell Therapies? A Study of Amniotic Fluid Preparations for Mesenchymal Stem Cells with Bone Marrow Comparison
Alberto J. Panero, DO*, Alan M. Hirahara, MD, FRCSC, Wyatt J. Andersen, ATC,
First Published 7, 2019 Research Article https://doi.org/10.1177/0363546519829034
Abstract
Background:
In vivo amniotic fluid is known to contain a population of mesenchymal stem cells (MSCs) and growth factors and has been shown to assist in healing when used as an adjunct in procedures across multiple medical specialties. It is unclear whether amniotic fluid products (AFPs) contain MSCs and, if so, whether the cells remain viable after processing.
Purpose: To determine whether MSCs, growth factors, and hyaluronan are present in commercially available Amniotic Fluid Products.
Study Design:
Descriptive laboratory study.
Methods:
Seven commercial companies that provide amniotic fluid were invited to participate in the study; 3 companies (the manufacturers of PalinGen, FloGraft, and Genesis AFPs) agreed to participate and donated AFPs for analysis. The AFPs were evaluated for the presence of MSCs, various growth factors relevant to orthopaedics (platelet-derived growth factor ββ, vascular endothelial growth factor, interleukin 8, bone morphogenetic protein 2, transforming growth factor β1), and hyaluronan by enzyme-linked immunosorbent assay and culture of fibroblast colony-forming units. These products were compared with unprocessed amniotic fluid and 2 separate samples of MSCs derived from human bone marrow aspirates. All groups used the same culture medium and expansion techniques. Identical testing and analysis procedures were used for all samples.
Results:
MSCs could not be identified in the commercial AFPs or the unprocessed amniotic fluid. MSCs could be cultured from the bone marrow aspirates. Nucleated cells were found in 2 products (PalinGen and FloGraft), but most of these cells were dead. The few living cells did not exhibit established characteristics of MSCs. Growth factors and hyaluronan were present in all groups at varying levels.
Conclusion:
The Amniotic Fluid Products studied should not be considered “stem cell” therapies, and researchers should use caution when evaluating commercial claims that products contain stem cells. Given their growth factor content, however, AFPs may still represent a promising tool for orthopaedic treatment.
Clinical Relevance:
Amniotic fluid has been proposed as an allogenic means for introducing MSCs. This study was unable to confirm that commercial AFPs contain MSCs.
Tags: amniotic fluid, arthritis, Bone Marrow Concentrate, Cartilage, cellular orthopedics, growth factors/healing enhancement, joint pain, mesenchymal stem cells, MSC, Orthopedic Surgeon, Osteoarthritis, regeneration, sports medicine, stem cell therapy
Mar 14, 2019
The basic principles behind the golf swing and the swing at home plate are not that much different. While the preferences may vary, when you break down the mechanics, there is similarity. Certainly there are differences between laying down a bunt and a 230-yard drive off the first Tee. The same differences are in play when putting is contrasted to the swing driving a 385-foot home run out of the park. In the several scenarios, the swing should look like one smooth, continuous motion that culminates with you holding a nicely balanced finish as the ball sails through the air. Within that motion however, is a series of techniques that each must be executed properly in order to produce the desired outcome.
Concentrating on golf swing mechanics, there is the Takeaway, Back swing, Transition, Impact, and Follow through. Continuing to explore the swing mechanics, backward movement of the shoulders and arms is followed by backward rotation of the spine, cocking of the hips, cocking of the wrists, timing, rotation of the pelvis, forward rotation of the spine, pushing and pulling of the arms and shoulders, guiding action and follow through.
Even if the physics behind my explanation is not perfect, the point here is that any pain and altered motion caused by injury or arthritis will affect your game. If you haven’t been able to play since last fall, now is the time to head out to the gym to catch up on strength training, stretching, with emphasis on spinal and pelvic rotation. Then there are the golf simulators and indoor driving ranges in and around Chicago.
If you experience pain in your muscles and joints along with limited motion, recent legislative changes in Illinois allow you direct access to the physical therapist. If after several sessions with the physical therapist, you haven’t realized the improvement you seek, it is time for an evaluation by an orthopedic surgeon. She or he, perhaps me, will complete a medical history and physical examination and review X-ray and MRIs of the effected anatomy. The end result of that intake may be a prescription for further PT, a prescription of pharmacologic management or in my case, a Regenerative Medicine/ Stem Cell procedure; that is a needle and not a knife.
I have documented in several recent scientific publications that Regenerative Medicine using either Bone Marrow Concentrate or Micro-fragmented Adipose tissue recovered by Liposuction will allow you to play 18 holes of golf this upcoming season. At times concentrated and then processed Platelets offer an opportunity for a patient afflicted with arthritis or limited by bodily injury to return to an active lifestyle and enjoy a full schedule of outdoor recreational pursuits. Please make note that my regenerative menu of services is based on your own cells and proteins that have been proven to work and meet FDA and FTC guidelines.
The weather forecast is improving and the sun was out today; the opening of both the baseball and golf season is only a about a week or so away. I say “Play ball.”
Tags: arthritis, Autologous Protein Concentrate, baseball, BMC, Bone Marrow Concentrate, cells, golf, injection, joint health, joint pain, lipogems, liposuction, micro-fragmented adipose, muscle injury, Orthopedic Surgeon, Osteoarthritis, pain, Physical Therapy, platelets, protein, PRP, regenerative medicine, sports medicine, stem cells, training
Feb 28, 2019
My column regarding ACL ruptures appeared last Friday. That afternoon, I received the following inquiry and comment from a reader, regarding the prognosis and possible early preventive interventions for a significant knee injury.
“I am one of relatively few patients who has had the Bone Marrow Concentrate treatment for a fully-torn (not-retracted) ACL tear and to date, I’ve had what I’d consider to be an amazing recovery. I read your latest blog post and just thought I’d let you know that I’m back to very aggressive skiing (including small but non-trivial jumps). However, I did want to ask, if you would be willing to comment, if there are actions or periodic diagnostics, you’d recommend to maximize the chances that I’m still happy skiing 10,20,30 years after the injury? I understand you probably can’t comment but nevertheless wanted to let you know I was also a real-life person who had a significant knee trauma with multiple surgical consults all agreeing it was fully torn and required surgery (to return to high-level skiing) and now have a fairly normal looking ACL in MRI (per independent radiologist) and am back to 100% with activities that require a lot of knee stability. I did do two rounds of same-day BMA reinjections and a bunch of platelet injections but no surgery.”
The answer is an orthopedic assessment at three-year intervals to look for markers of post traumatic osteoarthritis such as loss of terminal extension and asymmetrical flexion. The MRI is helpful in detecting moderate arthritic changes but the latest development, the needle scope, allows an orthopedic surgeon to directly examine the meniscus and cartilage in an office setting. The concern is post traumatic arthritis, cartilage defects that will progress, and meniscal damage not always seen on the MRI. Here are some thoughts on early intervention with Cellular Orthopedic and Regenerative Medicine options.
A recent Study Compared the Efficiency of Needle Arthroscopy Versus MRI for Meniscal Tears and Cartilage damage. Needle arthroscopy (NA) may be a less costly and more accurate option for diagnosis and treatment of meniscal tears and early onset post traumatic arthritis than MRI, according to a study published in the February issue of Arthroscopy. Researchers collected data on costs for care and accuracy, including procedures for both false-positive and false-negative findings well as private payer reimbursement rates. They compared outcomes using the global knee injury and osteoarthritis outcome score (KOOS). Patients were followed and evaluated over a two-year period.
There are several restorative options now available when conservative therapies for the treatment of knee degenerative processes, such as non-pharmacological interventions, systemic drug treatment, and intra-articular therapies offer only short-term benefits or fail. Before resorting to surgery; be aware that encouraging preliminary results have been reported using mesenchymal stem cells (MSCs), either alone or in association with surgery. My clinical published research documents success with using your Bone Marrow Concentrate for joint restoration and combating progression of posttraumatic arthritis. Additionally, I have published an article concerning another source for joint restoration, micro-fractured adipose tissue. The latter has created a huge interest in the context of cartilage regeneration due to its wide availability, ease to harvest and richness in mesenchymal cell elements within the so called stromal vascular fraction. Moreover, MSCs from adipose tissue are characterized by marked anti-inflammatory and regenerative properties, which make them an excellent tool for regenerative medicine purposes.
Tags: ACL tear, Adult Mesenchymal Stem Cells, arthritis, Arthroscopy, biologics, bone marrow, cartilage damage, cellular orthopedics, hip pain orthopedic surgeon, joint pain, joint restoration, knee pain, KOOS, meniscal tears, MSC, orthobiologic, Osteoarthritis, PRP, sports medicine, therapy, treatment