Feb 4, 2019
On Monday, the annual migration for attempts at the physical Restoration and Regeneration of the NFL players injured bodies began. While in the past, the losers would chant “wait ‘til next year”; very soon, the NFL winners and losers alike will take flight to Orthopedic Surgeons around the USA and world, on occasion, some will even find their way to my office, seeking both operative and non-operative repair of the injuries incurred over the last eight months. What I will offer is Regenerative and Restorative initiatives using either the patient’s bone marrow, circulating blood or body fat. While I use a needle and not a knife in my practice, at times it takes arthroscopy and open surgical procedures to assist the athlete in returning to play or extending a career. The fall NFL 2019 schedule is already on line; there is a sense of urgency. These attempts at restoring and regenerating anatomic and physical well-being are not limited to the professional football player. To the best of my recollection, it was Tiger Woods in 2008, who brought regenerative medicine to the attention of the American public. When in 2011, Kobe Bryant traveled to Dusseldorf, Germany for a highly publicized orthobiologic treatment of his arthritic knee, returning to play for another six seasons, he was soon after followed by the professional golfer Fred Couples, baseball player Alex Rodriguez, and NFL star Payton Manning. All returned to their respective sport and extended playing careers; many more have followed. Now Cellular Orthopedics, Regenerative Medicine and Joint Restoration are available around our country as well as at my office for professional, college, high school, amateur athletes and fitness enthusiasts of any age.
Orthobiologics and Cellular Orthopedics are a dynamic approach to body injury and arthritis using the individual’s own (autologous) platelets, molecules and proteins circulating in the blood (Cytokines and Growth factors), adipose tissue, or bone marrow to effect healing and eliminate pain. At this time, it is FDA Compliant to use such in the care and treatment of injury and arthritis as long as that which is to be used has been harvested from the patient herself or himself, not cultured or expanded, and not treated with additional agents. The successes are no longer merely anecdotal; there is an ever-increasing body of scientific evidence to validate the emerging discipline of Cellular Orthopedics. For instance, in my office, I integrate patient care with documenting outcomes and that has led to several recent scientific publications contributing to an evidence-based orthobiologics practice. You may find those publications and more at my web site www.sheinkopmd.com. To schedule a consultation call (312) 475-1893.
There is a way of still being an athlete and significantly reducing your risk of injury, take up esports. Marquette University is adding varsity esports, a competitive video gaming team in the fall of 2019. The team will have tryouts, coaches and regular practices just like any intercollegiate sport
Tags: arthritis, athletes, autologous, avascular necrosis, bone marrow, cellular orthopedics, cytokines, esports, Growth Factors, injury, joint pain, joint replacement, joint restoration, knee pain, meniscus tear, MSC, OA, orthobiologic, Orthopedic Surgeon, Osteoarthritis, Pain Management, pain reduction, patyon manning, platelets, PRP, sports injury, sports medicine, stem cells, superbowl, surgery, tiger woods, torn labrum

Dec 13, 2018
You may recall from my last several Blogs that The American Journal of Orthopedics published my paper in November: Safety and Efficacy of Micro-Fractured Adipose Tissue for Knee Arthritis. While surfing the internet this morning, I noted that many physicians are labeling the procedure a source of stem cells; it is not.
Lipogems is now U.S. Food and Drug Administration (FDA) approved for use in Orthopedics. The proprietary name is applied to a Micro-fragmented Adipose Tissue Transplant System that was the technology I introduced and monitored in a scientific clinical trial dating back three years leading to the publication. Federal regulators have now cleared the way for the device and technology that uses a patient’s own body fat (known clinically as adipose tissue) to assist in the healing process. Lipogems is attractive to orthopedic physicians because it is compliant with the latest FDA guidelines and is cleared for use in orthopedics. Unfortunately, clinics and physicians are erroneously, describing the procedure as a source of stem cells; I will emphasize again it is not. Even the Lipogems company uses term reparative and not regenerative.
The Power of Fat
When I grew up, my grandmother and mother fed me chicken soup for whatever ailed me. Many patients are looking for another option to major invasive surgery. Fat has many important cells and is easy to get from the patient’s body. Micro fragmented adipose tissue may be an option for patients who have tried physical therapy, nonsteroidal anti-inflammatory drugs, or steroid injections, and other treatments that have not provided enough relief.
In November 2017, the FDA finalized its rules guiding the use of Human Cellular and Tissue Products. The Agency reaffirmed that the Lipogems system meets the new guidelines’ criteria for minimal manipulation of the tissue, and that it is intended for homologous use. “Fat has been used for many years in support of the repair or replacement of damaged or injured tissue,” according to Dr. Arnold Caplan of Case Western Reserve University in Cleveland, Ohio. “Fat has a high concentration of reparative cells and is a very powerful tissue. How the fat is processed makes a huge difference on the quality of the tissue and if it meets the new FDA guidelines.”
To schedule an evidence-based consultation for your arthritic joint, call (312) 475-1893.
You may access my website at www.sheinkopmd.com
If you schedule before the end of the year, I will share my wife’s chicken soup recipe on request
Tags: arthritis, athletes, Clinical Studies, Clinical Trial. Mitchell B. Sheinkop, FDA, Interventional Orthopedics, knee pain, lipogems, Micro-fragmented Adipose Tissue Transplant, Osteoarthritis, stem cells

Dec 26, 2016
On October 28, 2013, I received IRB approval for a clinical trial with Regenexx Sciences, LLC as the sponsor and me as the Principal Investigator. The study, A Randomized Controlled Trial of Regenexx SD versus Exercise Therapy for Treatment of Knee Osteoarthritis with Historical Comparison to Total Knee Arthroplasty, was undertaken by me because of my recent “graduation” from joint replacement surgery to the new world of interventional orthopedics and because of my 37-year history as a joint replacement pioneer. Earlier this month, I was able to begin forwarding outcomes data to Regenexx in Broomfield, Colorado, for statistical tabulation. The results of this trial will not only impact what and how the Regenexx Network will make interventional recommendations, as the first and most comprehensive study of its kind, it will serve as the basis for comparison of all ongoing and future Regenerative Medicine methodologies for the care and treatment of the arthritic knee.
From Stem cells to Growth factors, the integration of our clinical research and clinical practice is having a major impact within the field of interventional orthopedics. Our results are allowing patients to return to activities they enjoy using a needle instead of a knife. I do not claim to be a cellular biologist but my network now allows me insight into the latest cellular advances. With the incorporation of the Abbott’s Ruby cell counting system into my clinical practice, I now customize the Bone Marrow Concentrate to the individual needs of a patient and thus not only quantitate but qualitate that which I inject into an arthritic joint.
Many Musculoskeletal injuries and certainly arthritis, do not heal with conservative management and historically required surgical intervention. The most contemporary method of effecting healing and regeneration is both Platelet Rich Plasma and Bone Marrow Concentrate. If you take a second look at the title of the clinical trial cited above, you will see the complete title ends with “Historical Comparison to Total Knee Arthroplasty”. The control group for the trial were patients with an arthritic knee in whom I had performed Total Knee Replacements during my surgical years. I am one of the few Orthopedic Surgeons who have experiences both in joint replacement surgery and interventional orthopedics. The majority of stem cell recipients have returned to activities they enjoy; the majority of Total Knee recipients are couch potatoes. When the numbers become available after statistical tabulation, I will post the data on my Blog.
Recently, I became aware of a relatively new web site www.Desirelist.com. The web site allows you to discover, capture and list all you may desire with a high probability of realizing your desires. So, I went on line and listed that which I want for my patients in 2017; namely, Internal Peace in a World at Peace. Where I can make a difference for those limited by arthritis of a major joint , and deliver on your desire for an improved quality of life is through Regenerative Medicine and Interventional Orthopedics.
Happy Chanukah, Merry Christmas and Happy and Healthy New Year
Tags: ACL Injury, arthritis, athletes, bone marrow, Clinical Trial. Mitchell B. Sheinkop, Growth Factors, Hip Replacement, Orthopedic Care, stem cells, treatment

Dec 1, 2016
Actually, that future started last week when we used a more aggressive PRP adjunct at the time of two Bone Marrow Concentrate/ Stem Cell interventions; one for an arthritic hip and the other, in an arthritic knee. More accurate and descriptive would be a Bone Marrow Concentrate/Adult Mesenchymal Stem Cell/ Hematopoietic Stem Cell/ Growth Factor Concentrate/Platelet Rich Plasma/Interleukin-1 Receptor Antagonist cellular orthopedic intervention to an arthritic joint but even I get confused, so I will stick to cellular orthopedics and Bone Marrow Concentrate.
It would seem from current Regenerative Medicine Science, that while concentrated and activated Platelet Rich Plasma alone has not been provided a predictable and reliable independent approach to arthritis, when aggressively used in conjunction with stem cell interventions, PRP significantly enhances the results in the short term. It will require another several years to determine if what we are seeing in the short term will continue to improve our outcomes in the long run. I am not waiting as concentrating and activating the platelets will cause no harm; and if there is the promise of long term benefits when used as an adjunct both at the time of the Bone Marrow collection, concentration and intervention as well as again in two to five days, there is no reason not to proceed.
What about the future? While we have been great advocates of counting cells at the time of the stem cell intervention, new tools are being introduced to allow us to better customize that which we inject after concentrating and processing of the bone marrow. We now will be able to get a more accurate count of that which is present in the concentrated and processed injectate prior to the intervention and add bone marrow or platelets if indicated.
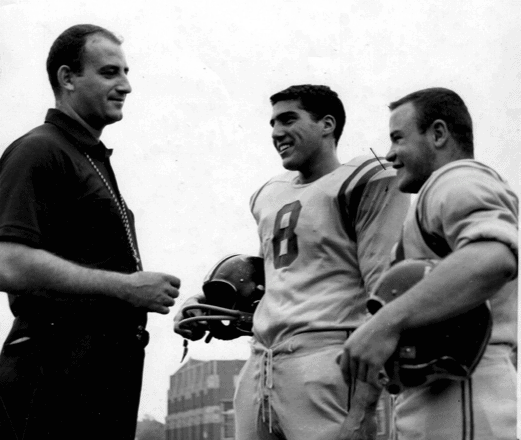
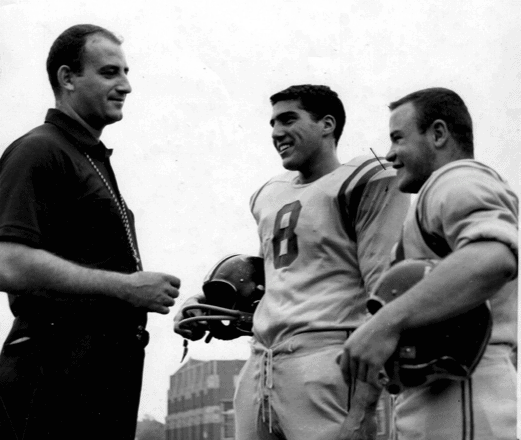
Are Mesenchymal Stem cells really Stem Cells? Professor Arnold Caplan of Case Western Reserve is widely considered the father of mesenchymal stem cells. He now takes the view that MSCs aren’t stem cells and that he should have never given them that name. He also believes that the primary function of these cells is paracrine, so he calls them “medicinal signaling cells”. To save you the trouble, paracrine is defined as “a form of cell-cell communication in which a cell produces a signal to induce changes in nearby cells.” I am not negating the importance of mesenchymal stem cells, rather I want the reader to better understand the role of each component involved with regenerative medicine. It was Professor Caplan’s prodding that in part is responsible for my having entered the discipline of interventional orthopedics. Long ago, we became friends as team mates of the Roosevelt High School championship football team in Chicago; and our professional paths, while parallel, he in basic orthopedic research while I chose orthopedic surgery finally crossed again five years ago.
To learn more about the basic science behind Cellular Orthopedics or to find out about how you might postpone or avoid a Total Joint replacement for an arthritic joint, schedule a consultation (312) 475 1893
Tags: arthritis, athletes, bone marrow, Bone Marrow Concentrate, cellular orthopedics, Clinical Studies, Concentrated Stem Cell Plasma, Growth Factor Concentrate, Growth Factors, Hematopoietic Stem Cell, Hip Replacement, Interleukin-1 Receptor Antagonist, knee arthritis, Mesenchymal Stem Cell, Mitchell B. Sheinkop MD, Orthopedics, Osteoarthritis, paracrine, Platelet Rich Plasma, Professor Arnold Caplan, PRP, Regenerative Pain Center, stem cells

Oct 20, 2016
Aging is known to contribute to a multitude of systemic changes including those of the musculoskeletal system leading to decreased health, mobility and function. Most changes in well-being are exacerbated by inactivity. It has been scientifically documented that physical activity and exercise may slow or even reverse these deleterious effects thereby improving health, mobility and function.
In particular, ligaments, tendons and joint capsules become stiffer with age as elastic fibers decrease and cross-links between collagen fibers increase. As connective tissue surrounding the joint changes, so too does the synovial fluid within the joint making movement more difficult. Not only do changes occur within the joint, they also occur in the muscles. The loss of muscle mass and strength also known as sarcopenia, increases with age. Then there is the fatty infiltration of muscle that comes with aging and lack of use.
Recognizing the value of Bone Marrow Concentrate derived Stem Cells, Cytokines and Growth Factors in dealing with his arthritic hip when the alternative was a joint replacement, seven months ago, a 58-year-old man underwent a cellular orthopedic intervention. Over the past many months, the patient committed himself to a minimum of 30 minutes a day, five days a week at moderate intensity aerobic exercise alternating with three days a week at vigorous intensity. In addition, he partook in resistance exercise a minimum of two days a week at a moderate high intensity focusing on 10 exercises at each session targeting most major muscle groups, with 10 to 15 repetitions for each exercise performed thus adding an additional 20 to 30 minutes to the commitment. Then there are the benefits of his additional flexibility and stretching. When this individual came to me at his first visit, his stated goals were to return to a high level of recreational enjoyment with a particular interest in ball room dancing. As of last week, he had reached those goals but he has no intention of failing to comply with his exercise prescription.
The obvious message of my Blog is to let you know I am unable to reach a desired goal without your commitment. I may introduce Stem Cells, Cytokines and Growth Factors into an arthritic joint but to reach your desired goal or delay or perhaps avoid a joint replacement, those many changes that occur with aging can be slowed and even reversed by a combination of cellular orthopedics and exercise.
If you want to learn about the evidence, schedule an appointment 312 475 1893
Tags: arthritis, athletes, Benefits and Risk, bone marrow, Bone Marrow Concentrate, Concentrated Stem Cell Plasma, Growth Factors, Hip, Hip Replacement, Interventional Orthopedics, joint replacement, Knee Pain Relief, Mature Athlete, Orthopedic Care, Orthopedic Surgeon, Orthopedics, Osteoarthritis, Pain Management, Regenerative, regenerative medicine, Regenexx, stem cells, treatment