Oct 18, 2018
We are speaking of stem cell therapy integrated with clinical research, and the resultant evidence-based stem cell intervention. Osteoarthritis is becoming more prevalent as I am seeing younger patients with arthritis as a consequence of sporting injuries such as ACL tears. The baby boomer population is experiencing accelerated onset of arthritis; their joints are prematurely aging in large numbers. At the same time, the master population is aging and living longer. As a result, I continually research biologic interventions to best address the ever-increasing number of those effected.
Why should a patient choose an orthopedic surgeon to manage their Osteoarthritic related symptoms and functional impairment? Our world is evidence based.
Study Observes Better Outcomes for OA Patients Treated by an Orthopaedic Specialist
In a retrospective study published online in BMC Musculoskeletal Disorders, shoulder osteoarthritis (OA) patients received faster and more invasive treatment when they received a new diagnosis from an orthopaedic specialist (OS) versus a nonorthopaedic physician (NOP). Patients with shoulder OA (n = 572) received care from either an OS (n = 474) or NOP (n = 98) on the date of their index shoulder visit. OS patients received their first treatment significantly quicker than the NOP cohort (16.3 days versus 32.3 days, respectively). The OS group also had higher rates of operative treatment within one year following their initial visit.
Study: Patients Report Similar Improvements for Nonobstructive Meniscal Tear with PT and Early Surgery
Physical therapy (PT) may not be inferior to early operative treatment of arthroscopic partial meniscectomy (APM) for improving knee functionality in patients with nonobstructive meniscal tears, according to a study published online inJAMA. The randomized clinical trial included 321 patients with nonobstructive meniscal tears aged 45 to 70 years who were treated at nine hospitals in the Netherlands between July 17, 2013, and Nov. 4, 2015. Patients were treated with APM (n = 159) or a predefined PT protocol (n = 162) that included 16 exercise therapy sessions over eight weeks. PT sessions focused on coordination and closed kinetic chain strength exercises. At 24-month follow-up, knee functionality in the PT group improved by 20.4 points compared to 26.2 points in the APM group. The difference did not exceed the noninferiority margin.
In order to maximize the benefits, Orthobiologics, that is stem cell therapy must be integrated with clinical research, and the resultant evidence-based stem cell intervention followed long term. In my practice, I am researching biologic interventions to address the ever-increasing number of those effected, not one and done. To learn more or schedule a consultation, Call (312)475-1893. You may visit my web site and read my blogs at www.sheinkopmd.com
Tags: ACL tear, arthritis, Cartilage, cellular orthopedic, joint pain, joint replacement, knee pain, MCL tear, meniscus tear, menisectomy, orthobiologics, orthopedic surgen, Osteoarthritis, Physical Therapy, PRP, regenerative medicine, stem cell

Oct 5, 2018
After reviewing a CT scan of the right knee where a Total Knee Replacement had been done provided by a patient who sought my opinion for stem cell treatment of her arthritic left knee, I called her to discuss the possible reasons that the right Total Knee Replacement that she had undergone over ten years ago was never satisfactory. At the time of the right TKR for arthritis, she had elected for what seemed at the time as a logical intervention for a painful, arthritic, right knee. The outcome was at first complicated by a lot of postoperative swelling and pain; at one-year post-operative, the patient had never been pain-free nor had she ever regained her preoperative range of motion and that adverse outcome has persisted for over ten years. Fast forward a decade and the right knee has continued to be a source of pain and limited motion; so much so that the patient decided to seek consultation for a Stem Cell treatment for her now arthritic left knee.
Her first question was basically “does stem cell therapy for knees work?”. Our data collected on patients treated in this office over the past six years, since I started my practice, is compatible with an 85% patient satisfaction rate. We have not recorded one complication. To be forthright, not every patient has a perfect result; but the vast majority experience marked reduction in pain, increased motion and a significant improvement in functional capacity. Unlike a failed outcome of a Total Knee Replacement, our stem cell injections may be repeated at anytime if the benefits of the initial intervention do not last.
When it comes to the cost of a stem cell intervention, while the Total Joint Replacement is more often than not covered by some type of insurance, our fee schedule is in keeping in line with the deductible a patient has to pay out of pocket for the major surgery. If you do the math and additionally compare the risks and benefits of a stem cell intervention with a total knee replacement, you will note:
- Remote to little risk of complication with a stem cell procedure
- Comparable cost comparing my charges for a stem cell intervention with the inherent deductible obligation for a Total Joint Replacement
- Rapid recovery with a stem cell intervention versus the risks of an adverse outcome as experienced by the patient seeking consultation for stem cells
To seek consultation call (312) 475-1893. You may visit my website at WWW.sheinkopmd.com
Tags: cellular orthopedics, ct scan, joint health, joint replacement, knee pain, knee replacement, Osteoarthritis, regenerative medicine, stem cell treatment, TKA

Jul 19, 2018
The argument frequently advanced by orthopedic surgeons in response to a patient’s inquiry concerning stem cells for arthritis is that it is too early, there is not enough research, It is better to have a major surgical procedure. For those of you who have read my blog or have sought orthopedic consultation in my office, I have emphasized that my recommendations are evidence based. Each patient, for whom I have completed a cellular orthopedic intervention for arthritis, has been entered into a registry or clinical outcomes data base, IRB approved. Just as I pioneered the integration of clinical care with clinical research over 37 years as a joint replacement surgeon, so too do I now partake in the growth and development of the clinical pathways for regenerative medicine.
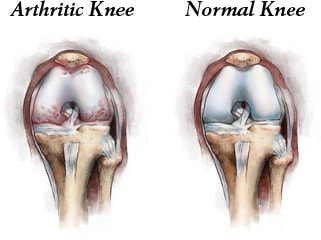
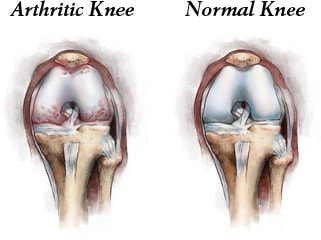
Last month, I exhibited a poster at a large regenerative medicine meeting wherein I shared my preliminary outcomes and thus educated other professionals using Intraarticular and Subchondral Bone Injection of Autologous Bone Marrow Concentrate and General Fluid Concentrate for Osteoarthritic Knees-A Prospective Clinical Study. Osteoarthritis is an organ disease that affects most structures of joints including cartilage, synovium and subchondral bone. Pathology in subchondral bone contributes to the initiation, progression and pain of Osteoarthritis. In previous European studies, the injection of autologous bone marrow concentrates into bone supporting the joint significantly relieved pain and improved function of the affected knee. The preliminary outcomes in the study that I presented via a poster exhibit, investigated the effectiveness of injections of Bone Marrow Concentrate with General Fluid Concentrate (Growth factors), into both the knee joint and the subchondral bone. The study recorded all the standard Endpoints I had previously used in joint replacement clinical outcomes trials.
Bone Marrow was collected from the pelvis and a filtration system allowed for concentration of Mesenchymal Stem Cells, Platelets, Precursor Cells and Growth factors such as A2M, IRAP, EGF, PDGF, TNF-B blocker, etc. After preparation, a mixture of Bone Marrow Concentrate and Growth factor Concentrate was injected into the bone (subchondral) and into the joint.
In the study, all patient injections went well and there were no complications. The Preliminary Results documented diminished pain and improved function. We concluded that injection of Bone Marrow Concentrate and Growth factor Concentrate into both the subchondral bone area and joint cavity significantly improved function of the affected knee joints and significantly reduced joint pain. While there are many stem cell providers to be found because of their marketing, choose the center of excellence in Cellular Orthopedics that is evidence based.
Call to schedule a scientific based consultation from an orthopedic surgeon 1 (312) 475-1893.
You may access my web site at www.SheinkopMD.com.
Tags: avascular necrosis, bone lession, bone marrow, Cartilage, cellular orthopedics, clinical study, Growth Factors, IRAP, joint pain, joint replacement, knee pain, knee replacement, meniscus tear, Osteoarthritis, platelets, PRP, regenerative medicine, sports medicine, stem cells, subchondral bone
Jun 28, 2018
For those unfamiliar with the designation, it is for the one who makes public pronouncements though I don’t dress elaborately by tradition nor do I carry a handbell saying “Oyez, oyez” (hear ye, hear ye)
“Twenty percent of knee replacement patients are not happy with their total knee replacements.” –Orthopedics, This Week Tuesday, June 12, 2018
“Arthroscopy for knee OA did not reduce or delay the need for a TKA” – Journal Arthroscopy. Sept 23, 9 2017
“Dr. Atul Gawande, a surgeon who was named this week to head the company being formed by Amazon, Berkshire Hathaway and JPMorgan Chase to trim employee healthcare costs, on Thursday cited surgery as the single biggest U.S. healthcare cost and said there are ways to both cut costs and improve patient care” “We need to act through data tracking … to see when treatments are benefiting and when they are not,” Gawande said. – Headline News Now June 25, 2018
There is an appropriate time and place for a joint replacement; a symptom such as pain in the knee should not be the solitary indication. Neither should every patient with a joint complaint be told by a surgeon “you have bone on bone and need a joint replacement”. My office evaluation before I make an evidence-based outcomes recommendation includes a history and physical before I look at the images. Joint range of motion is equally important as is the review of symptoms prior to reviewing your images for determining if I can help you postpone a joint replacement though my menu of Regenerative and joint Restoration alternatives or whether you should proceed to a total joint replacement. Please be reminded that before I evolved into my present approach to musculoskeletal afflictions, I was an orthopedic surgeon at a major medical center where I headed the joint replacement program for many years. Every patient who goes to a physician is not necessarily an automatic candidate for a procedure offered by that physician. Yesterday, I submitted an application for an FDA monitoring of one of our newest offerings and a good deal of the application was not only based on the scientific basis but the inclusion and exclusion criteria.
There is a time and place for doing something or doing nothing. To determine what is in your best interest, call for a consultation (312) 475-1893 or visit one of my two websites; www.sheinkopmd.com or www.Ilcellulartherapy.com
Tags: Arthroscopy, Dr. Atul Gawande, Headline News Now, joint pain, joint replacement, knee arthroscopy, knee pain, knee replacement, knee replacement failure, Orthopedic Surgeon, Orthopedics, Restoration alternatives
Jun 22, 2018
My regenerative and restorative Cellular Orthopedics practice is for the most part, evidence based. By that I mean, the outcomes data collected over these past five years regarding the several thousand patients with skeletomuscular afflictions that I have treated with a selection of alternatives using a needle and not a knife is generally based on regenerative and restorative interventions. While not everyone has experienced a dramatic change in symptom relief and functional improvement, many have. The statistical outcomes evidence follows a bell shaped curve with some experiencing immediate improvement as I have in both my hips and knees, while most take several weeks or longer with a continuing improvement up to 18 months post intervention. While it is true that five percent of patients are not satisfied after several years and have gone on to a joint replacement, 95% of my patients are well satisfied and have returned to, or never quit doing what they love.
At the onset of my cellular orthopedic initiative, the interventions were solely based on Platelet Rich Plasma options and Bone Marrow Concentrate; today, our menu of services can be customized so as to meet the needs of all seeking to improve the quality of life and avoid a major surgical procedure. Not only can I concentrate PRP as needed, I can customize the concentration to meet a patient’s particular needs using hemo-analysis. Bone Marrow Concentrate rich in Adult Mesenchymal Stem cells, Platelets, Growth Factors and Precursor Cells is still the foundation of my practice, however for the past year, I am able to offer a Platelet Concentrate derived Growth Factor and Protein Solution option when indicated.
Then there are those whose co-morbidity or prescription medication dependency excludes them from the aforementioned autologous choice of options. As of this upcoming Tuesday, I have acquired an intervention technology that will help patients seeking to a void a total joint replacement who are not candidates for existing regenerative medial offerings. There are many reasons to explain a 5% failure rate including genetic cartilaginous variations, any bell shaped curve will have a small number who don’t pass the final examination. Incidentally, if and when such occurs, I offer another intervention frequently at no charge or certainly at a discounted rate.
Should you want to learn more or schedule a consultation, call
(312) 475-1896. You may visit my web site where you will find the webinar at www.Ilcellulartherapy.com.
Tags: bone marrow, cellular orthopedics, Growth Factors, Hip pain, joint pain, joint replacement, knee pain, Mesenchymal Stem Cell, Osteoarthritis, platelets