Nov 16, 2016
This week, I am repeating stem cell/growth factor interventions in two patients; one with arthritis of the
hip, and the other with osteoarthritis of both knees. Four years ago, at the initiation of my interventional
orthopedic practice, I spoke of adult mesenchymal stem cells alone but now we know that Bone Marrow
Concentrate has in addition to the adult mesenchymal stem cells, hematopoietic stem cells, growth
factors and platelets all playing a role in managing the symptoms and the altered functional impairment
attributable to osteoarthritis. The outgrowth is in new speak; namely, Bone Marrow Concentrate and not
just mesenchymal stem cells. When the two patients I alluded to were initially cared for, we had not yet
gained the understanding of the importance of platelets in the regenerative process. Platelets contain
the growth factors and those growth factors are responsible, in addition to Mesenchymal and
Hematopoietic Stem Cells, for regulating cartilage well-being. By having become aware of the
contribution following concentrated platelet rich plasma in conjunction with the bone marrow
concentrate intervention, I believe we are already seeing improved outcomes.
As well, subchondroplasty has been added to our menu of services and the latter is proving very
beneficial in the knee. To refresh your knowledge base, subchondroplasty is a procedure popularized in France where in bone marrow concentrate is injected into the bone marrow adjacent to a joint at the
same time that the stem cell, growth factors and platelet containing concentrate is intervention of the
joint itself is being completed. The value of intervening into the bone supporting the joint is the fact that
there is communication between the joint itself and the supportive subchondral environment. I have
addressed Adult Mesenchymal Stem Cells many times in previous Blogs as the orchestrater of the
healing process. Now we know that Hemopoietic Stem Cells from the marrow contribute as well. Growth
Factors such as Interlukin-1 Receptor Antagonist Protein (IRAP) are present in bone marrow and
circulating blood; It was IRAP alone that extended the professional basketball career of Kobe Bryant by
seven years for an arthritic knee. With an improved means of extracting and activating the growth
factors contained in platelets, the two patients I introduced in the opening sentences of this blog should
enjoy a very satisfactory return to function and recreation.
Interventional Orthopedics is a dynamic process and I continue to learn from the integration of clinical
research and my clinical practice. On Thursday, I will host two very interested scientists dedicated to
customizing biologic preparations and together we will explore how to further leverage scientific
advancements in creating autologous biologic preparations thereby optimizing the practice of
Regenerative Medicine.
Call 312 475 1893 to schedule your consultation
Tags: arthritis, bone marrow, Clinical Trial. Mitchell B. Sheinkop, Concentrated Stem Cell Plasma, Growth Factors, Hematopoietic Stem Cells, Interlukin-1 Receptor Antagonist Protein, IRAP, joint replacement, Osteoarthritis, Platelet Rich Plasma, PRP, Regenerative Pain Center
Oct 6, 2016
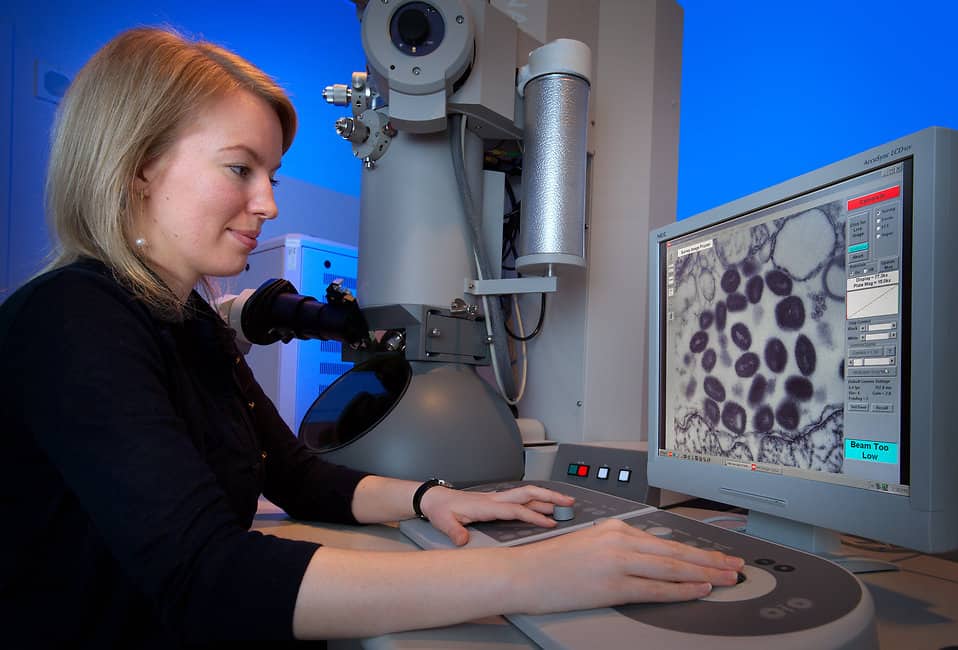
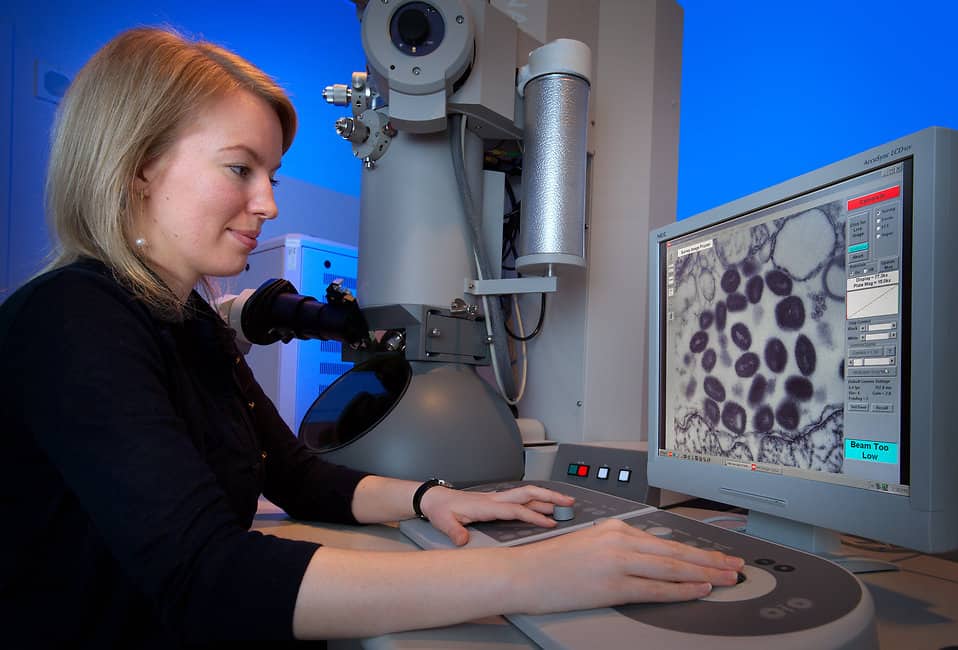
“Growth factor, any of a group of proteins that stimulate the growth of specific tissues. Growth factors play an important role I promoting cellular differentiation and cell division,” and they occur in bone marrow as well as your circulating blood.
“When investigators began studying the effects of biological substances on cells and tissues in culture, they discovered a group of peptide-hormone-like substances that were distinct from any previously known hormones. Because these substances were active in stimulating the growth of cells and tissues, they were called growth factors. Some growth factors are similar to hormones in that they can be secreted into the blood stream, which carries them to their target tissues. However, whereas the production of hormones is limited to glandular tissue, growth factors can be produced by many different types of tissue” and cells for that matter.
When a patient presents for a Bone Marrow Concentrate procedure for an arthritic joint in order to prevent, perhaps even avoid a joint replacement, the understanding to date is that it will be Mesenchymal Stem Cell that will serve as the key factor in reducing pain, increasing motion, improving function and influencing the progression of arthritis. The latter is only partially true but fails to address the role Growth Factors play in Cellular Orthopedics (Regenerative Medicine). When your orthopedic surgeon tells you that Stem Cells won’t work for your arthritis, schedule your joint replacement, that physician doesn’t understand that Stem cells are only part of what Bone Marrow concentrate provides us in assisting the patient with an arthritic joint, return to an active life style without surgery.
We now have several proprietary means of not only concentrating adult Mesenchymal Stem Cells but Growth Factors as well when addressing your arthritic joint with Bone Marrow Concentrate. While stem cells may be impacted by age, Growth Factors do not seem to be adversely impacted accounting for several recent successes with patients in their 90s. Since we have been concentrating stem cells with growth factors and combining the approach to the joint with subchondroplasty, we continue to document improving outcomes
Tags: arthritic pain, arthritis, arthritis treatment, Bone Marrow Concentrate, Concentrated Stem Cell Plasma, Growth Factors, Hip Replacement, joint replacement, Mesenchymal Stem Cell, Orthopedic Surgeon, Osteoarthritis, regenerative medicine, Regenerative Pain Center, stem cell treatment
Feb 8, 2016
Every week, I receive updates via brochures and journals concerning the clinical and basic science orthopedic research being done around the country at the various university medical centers. I like to read them to understand how Cellular Orthopedics is emerging and is being accepted in academic institutions. When I retired from Rush and joint replacement surgery five years ago, my colleagues had a very jaundiced view of my new endeavors telling me and then my patients that Regenerative Medicine was unproven, was ten years away, and was not a reasonable alternative to a joint replacement. It is with great pleasure that I am able to announce the American Academy of Orthopedic Surgery Surgical Skills update will include a three day course next month on Articular Cartilage Restoration: The Modern Frontier, as a continuing educational initiative. The title of one particular lecture really caught my attention Move-Over PRP/Viscosupplementation: Stem cells are in and why.
Taking it a step further, the latest bulletin from Jefferson Medical College’s department of orthopedic surgery reviews the basic science being done in the Laboratory of Theresa Freeman, PhD, Associate Professor of Orthopedic Surgery. “The development of Osteoarthritis can often be attributed to a trauma that occurs in youth, which begins the slow degeneration of cartilage. By reducing cartilage damage immediately after an injury, the development of osteoarthritis can be dramatically slowed.”
I have been making the case for an affirmative stem cell intervention every time an anterior cruciate surgical repair takes place or for that matter, when an individual undergoes an arthroscopic procedure. Two weeks ago, I completed a Bone Marrow Aspirate Concentrate Stem cell procedure three weeks after a young middle aged man had undergone micro fracture for a cartilage defect on the weight bearing part of his femur at the knee. On Friday, I scheduled a 72 year old gentleman for a stem cell procedure ten days after he had undergone arthroscopic surgery for a degenerative tear of his medial meniscus during the course of which degenerative changes were documented in the weight bearing zone at the inner compartment of his knee.
A webinar is scheduled by the American Academy of Orthopedic Surgeons next month in order to introduce its orthopedic membership to what may be possible through Cellular Orthopedics. I have already advised you about the Continuing Education Course next month on Articular Restoration. The orthopedic academy membership is only now being introduced to what I have been practicing for almost four years. There are now close to 750 patients in my data base who have undergone Cellular Orthopedic procedures for arthritic joints to relieve pain, increase function and avoid, certainly postpone a joint replacement. On Saturday, I am headed out to Colorado to ski with family for a week. For readers of my blog, you may recall I have undergone a regenerative procedure for my left knee. While I am realistic and I don’t dwell on being who I used to be, I believe anything is possible at any age. If you want to continue or possibly return to skiing, biking, hiking, climbing, fly fishing, skating, fitness, etc, and the limitation is arthritis, schedule a consultation
847 390 7666
Tags: ACL Injury, arthritis, athletes, Benefits and Risk, bone marrow, Bone Marrow Concentrate, Hip, Hip Replacement, Interventional Orthopedics, joint replacement, Knee, Knee Pain Relief, Mature Athlete, medicine, Microfracture surgery, Orthopedic Care, Orthopedic Surgeon, Orthopedics, Osteoarthritis, Pain Management, Regenerative, Regenerative Pain Center, Regenexx, stem cells, treatment

Nov 5, 2015
My last Blog brought you greetings and discussed some of the issues reviewed at the first meeting of the Interventional Orthopedic Foundation. This not for profit foundation was founded to help facilitate the transfer of scientific regenerative medicine developments into clinical practice. One challenge is how to improve the outcomes of what is now the gold standard of Interventional Orthopedics, Bone Marrow Aspirate Concentrate in managing arthritis of major joints. We seek to see longer effect and better results. While there are all kinds of claims being made for amniotic fluid concentrate and adipose (fat) derived stem cells, as of now, there is no data to support said claims.
I have played a large role in documenting the success of Bone Marrow Concentrate intervention for arthritis. Now I want to see if I can improve those results. At the Interventional Orthopedic Foundation meeting, various means of improving outcomes were discussed including, hyperbaric oxygen, ultrasound, lasers, ultraviolet light and finally, electro-stimulation. I was reminded of a study in which I was involved five years ago using an electronic pulse joined to a knee brace to try to regenerate cartilage. The study was based on animal models who when subjected to an electronic pulse grew cartilage. It occurred to me that the answer to improving the quantity and the quality of a Bone Marrow Aspirate Concentrate/ Stem cell intervention for an arthritic knee might be the pulsed brace. If every patient who undergoes a stem cell intervention for arthritis is prescribed a brace post treatment, since we know that the pulse is safe and potentially helpful, why not add the pulse to the post intervention protocol. To that end, I am happy to announce the introduction of this methodology to our post intervention protocol via a clinical trial starting in December
We will follow each patient for up to a year with our standard clinical objective and subjective means and periodic X-Rays with no added fiscal burden to the patient. The results of this study will then be presented to the 2016 meeting of the Interventional Orthopedic Foundation as I continue to integrate patient care with research. There is no question that patients who wore the brace and used the pulse for arthritis without stem cell intervention in the past were improved; imagine the potential leap forward by adding the pulse to the brace after a Bone marrow Aspirate Concentrate/ Stem Cell intervention.
Tags: arthritis, athletes, Benefits and Risk, Bone Marrow Concentrate, Clinical Studies, Clinical Trial. Mitchell B. Sheinkop, Hip Replacement, Interventional Orthopedics, joint replacement, Knee, Mature Athlete, medicine, Orthopedic Care, Orthopedics, Osteoarthritis, Pain Management, Pilot Study, Regenerative, Regenerative Pain Center, Regenexx, Regenexx-SD, stem cells, treatment

Sep 17, 2015
In the last week, I have become aware of four companies developing new regenerative medicine product for Musculoskeletal Care of the Aging Athlete. What I find extremely interesting is the fact that three years ago, when I entered the practice of using bone marrow aspirate concentrate in an attempt to postpone or possibly avoid a joint replacement in an arthritic knee or hip, the orthopedic community was very critical telling patients that regenerative medicine was still ten years away. Fast forward three years and four new initiatives into the emerging field of regenerative medicine have come to my attention; underwritten by orthopedic surgeons or companies that have produced prosthetic joints for over 30 years. All of the product in development has not yet been approved by the FDA and many developing products are still being tested in Europe. What we at the Regenerative Pain Center offer is within FDA guidelines and approved by all regulatory agencies of the government. At the same time, I am very much aware of what is taking place nationally and internationally; when a newer regenerative medicine product is made available and FDA approved, we at the Regenerative Pain Center will be aware and closely evaluate as to whether it should be incorporated into our service line.
Let me be candid, our success rate is not 100 per cent. There have been three or four hip patients that have not provided the outcome the patient sought or that I hoped to provide; namely, avoidance of a hip replacement. On the other hand, the vast majority of hip bone marrow aspirate concentrate procedures are still allowing the patient a very full return to activities with about 70% percent patient satisfaction at a minimum of one year. When it comes to those who sought help for an arthritic knee, we have done even better with an 85% patient satisfaction outcome at a minimum of one year. Several of those patients had reached a plateau at six months but realized a marked improvement in the pain score with a Platelet Rich Plasma refresher. When a patient elects to under go a bone marrow aspirate concentrate hip or knee intervention at the Regenerative Pain Center, that patient may be assured that what we are doing is based on FDA guidelines and our clinical outcomes research. In addition, each patient should recognize that Regenexx continually statistically reviews our outcomes data. Last week, we recognized that those who underwent Cellular Orthopedic interventions for an arthritic knee did best when the cell count of mononuclear cells exceeded 400 million. Be aware that we count the cells in every Regenerative Medicine procedure. Our approach is no longer “this is the way we do it.” Our approach is based on experience and outcomes research, the same that I used in a long joint replacement career.
Tags: arthritis, athletes, Benefits and Risk, Bone Marrow Concentrate, Concentrated Stem Cell Plasma, FDA, Hip, Hip Replacement, Interventional Orthopedics, joint replacement, Knee Pain Relief, Mature Athlete, Orthopedic Care, Orthopedics, Osteoarthritis, Pain Management, Platelet Rich Plasma, Regenerative, Regenerative Pain Center, Regenexx, stem cells, treatment