Feb 28, 2019
My column regarding ACL ruptures appeared last Friday. That afternoon, I received the following inquiry and comment from a reader, regarding the prognosis and possible early preventive interventions for a significant knee injury.
“I am one of relatively few patients who has had the Bone Marrow Concentrate treatment for a fully-torn (not-retracted) ACL tear and to date, I’ve had what I’d consider to be an amazing recovery. I read your latest blog post and just thought I’d let you know that I’m back to very aggressive skiing (including small but non-trivial jumps). However, I did want to ask, if you would be willing to comment, if there are actions or periodic diagnostics, you’d recommend to maximize the chances that I’m still happy skiing 10,20,30 years after the injury? I understand you probably can’t comment but nevertheless wanted to let you know I was also a real-life person who had a significant knee trauma with multiple surgical consults all agreeing it was fully torn and required surgery (to return to high-level skiing) and now have a fairly normal looking ACL in MRI (per independent radiologist) and am back to 100% with activities that require a lot of knee stability. I did do two rounds of same-day BMA reinjections and a bunch of platelet injections but no surgery.”
The answer is an orthopedic assessment at three-year intervals to look for markers of post traumatic osteoarthritis such as loss of terminal extension and asymmetrical flexion. The MRI is helpful in detecting moderate arthritic changes but the latest development, the needle scope, allows an orthopedic surgeon to directly examine the meniscus and cartilage in an office setting. The concern is post traumatic arthritis, cartilage defects that will progress, and meniscal damage not always seen on the MRI. Here are some thoughts on early intervention with Cellular Orthopedic and Regenerative Medicine options.
A recent Study Compared the Efficiency of Needle Arthroscopy Versus MRI for Meniscal Tears and Cartilage damage. Needle arthroscopy (NA) may be a less costly and more accurate option for diagnosis and treatment of meniscal tears and early onset post traumatic arthritis than MRI, according to a study published in the February issue of Arthroscopy. Researchers collected data on costs for care and accuracy, including procedures for both false-positive and false-negative findings well as private payer reimbursement rates. They compared outcomes using the global knee injury and osteoarthritis outcome score (KOOS). Patients were followed and evaluated over a two-year period.
There are several restorative options now available when conservative therapies for the treatment of knee degenerative processes, such as non-pharmacological interventions, systemic drug treatment, and intra-articular therapies offer only short-term benefits or fail. Before resorting to surgery; be aware that encouraging preliminary results have been reported using mesenchymal stem cells (MSCs), either alone or in association with surgery. My clinical published research documents success with using your Bone Marrow Concentrate for joint restoration and combating progression of posttraumatic arthritis. Additionally, I have published an article concerning another source for joint restoration, micro-fractured adipose tissue. The latter has created a huge interest in the context of cartilage regeneration due to its wide availability, ease to harvest and richness in mesenchymal cell elements within the so called stromal vascular fraction. Moreover, MSCs from adipose tissue are characterized by marked anti-inflammatory and regenerative properties, which make them an excellent tool for regenerative medicine purposes.
Tags: ACL tear, Adult Mesenchymal Stem Cells, arthritis, Arthroscopy, biologics, bone marrow, cartilage damage, cellular orthopedics, hip pain orthopedic surgeon, joint pain, joint restoration, knee pain, KOOS, meniscal tears, MSC, orthobiologic, Osteoarthritis, PRP, sports medicine, therapy, treatment
Jan 5, 2018
If you read my blog posting last week, you would have learned that I personally underwent a cellular orthopedic intervention to both of my knees on Wednesday, 12/27. The symptoms attributable to my own osteoarthritis had progressed to a degree that I was becoming limited in my recreational profile. While there indeed was a response to anti-inflammatory medications, every time I am reminded of the potential complications of NSAIDS, I become medication adverse. This led to the injection into both of my knees of an Autologous Protein Concentrate (APC) with the hope of treating my pain and slowing the progression of cartilage degradation and destruction of my knees.
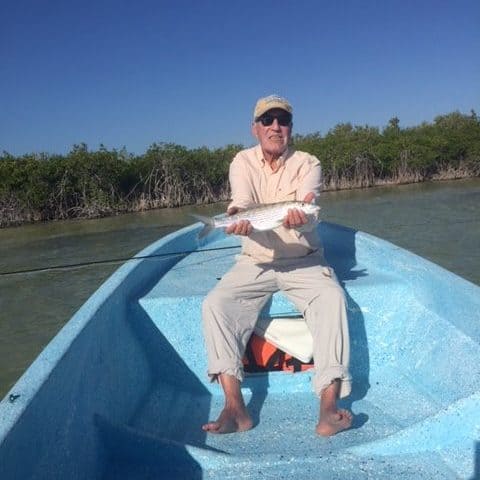
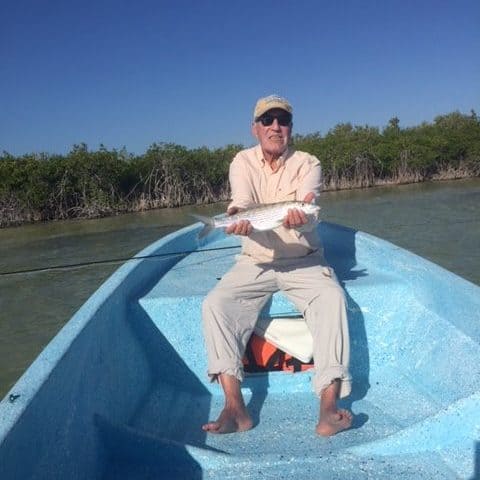
The process used was a cell-concentration system which concentrated my own anti-inflammatory cytokines and anabolic growth factors. Pioneered in Europe, an ever-increasing number of professional athletes have been prolonging their careers by accessing this treatment. I have waited over five years for the Autologous Protein Concentrate methodology to become available in the United States; three weeks ago, I was granted access. To date, my pain secondary to knee osteoarthritis is not only reduced but gone; I can only hope it stays that way. My function is significantly improved as evidenced by an ability to have pursued my fly fishing passion chasing bone fish with my wife, daughter-in-law and son for three days in Ascension Bay, Mexico, over the New Year weekend. For those unfamiliar, bone fishing requires a continued down and up to a platform on the front of a three-man boat with prolonged standing while balancing. At times, I climbed out of the boat and waded through the flats for 30 to 45-minute intervals until it was time to change locations. Since returning home on January 1, I have been able to return to my fitness profile without restriction previously afforded by my Osteoarthritis generated symptoms and limitations.
As in any and all treatments, a patient must be given informed consent and be warned both of the benefits and risks; so, I will let you in on an adverse event in my early outcome. Owing to the increased activity attributable to the diminution of my pain and increased functional capacity resulting from my initial response to the Autologous Protein Concentrate intervention, instead of climbing down from the fly fishing platform in the front of our boat when it was time to trade places with my wife, I jumped down. In so doing, I kicked the rod holding rack and fractured the fifth toe on my left foot, the pinky toe. Though a bit of a nuisance, it is not too great a price to pay for the relief and improved function of my knees.
To learn more, call my office and schedule an appointment; as I haven’t yet updated my web site with an explanation of the Autologous Protein Concentrate intra-articular injection for treatment of knee osteoarthritis (312) 475-1893.
Tags: anti-inflammatory, arthritis, Autologous Protein Concentrate, cytokines, Growth Factors, Hip Replacement, horse, injection, Interventional Orthopedics, joint replacement, Knee Pain Relief, Osteoarthritis, Pain Management, regenerative medicine, rheumatoid arthritis, treatment, treatment of equine lameness

Oct 20, 2017
Well, it is really an internal debate as to whether I should have a concentrated platelet rich plasma procedure or a bone marrow concentrate procedure as I get ready for the upcoming ski season. While it is true that I exercise five to six days a week rotating between outdoor cycling, strength training and rowing, the demands of skiing on the knees are such that I need to rethink my approach. I share this personal flow of conscience to provide guidance and council for readers of this blog. As for so many of us senior recreational participants, each activity has unique demands so we must anticipate each activity from a separate approach. While generalized fitness improves the quality of life and even well-being, maybe even prolonging life, if you want to ski with arthritic knees, now is the time to plan ahead.
Let me share with you my plan based on an observation of the outcomes in over 1500 patients in whom I have intervened with Cellular Orthopedic alternatives over the past five years. In the next several weeks, I will undergo a concentrated PRP intervention ultrasound guided into both of my knees. I will be using the upgraded methodologies for preparation of injectate and customize the PRP with our soon to be activated cell counter. This will provide me with a 20x dosage over that which has been available up until the present; and yes, I too have to pay for the methodology. I will then wait until mid-December, and if I am not satisfied, I will undergo a Bone Marrow Cell Concentrate procedure for both of my knees.
Below are two reasons received in the last 48 hours as to why I believe Cellular Orthopedic is exciting:
“My uber-condensed version, though, is that on almost all days in the last 8 months, I’ve had virtually no knee pain with daily activity. That’s a massive improvement from even the 12-month follow-up visit. I first started to suspect things were improving at about 10 months post-op. At 12 months, I was hopeful but still skeptical. At 14 months things, rapidly improved and have mainly remained there ever since. So, on the whole, I’m vastly improved. I suppose any number of factors could have contributed to that improvement, but Regenexx certainly seems to have helped tremendously.”
“Attended the company golf outing this past weekend. Last year I was concerned so I took an Advil before we started and ended up taking another halfway through the 18 holes. The last four holes I didn’t even leave the cart (to sore/tight to get in and out).
This year I fully intended to bring the Advil again but forgot it. Turned out I did not need it. Finished the 18 holes like nothing. Felt fine after and the next day.
Believe we can consider this a win!!!!”
Do you want to enjoy relief from arthritic symptoms and limitations?
Call 312 475 1893 to schedule a visit or visit my website to watch my webinar www.Ilcellulartherapy.com
Tags: arthritis, Clinical Trial. Mitchell B. Sheinkop, Knee Pain Relief, Orthopedics, treatment

Aug 31, 2017
The Food and Drug Administration is cracking down on “unscrupulous” clinics selling unproven and potentially dangerous treatments involving stem cells.
Hundreds of clinics around the country have started selling stem cell therapies that supposedly use stem cells but have not been approved as safe and effective by the FDA, according to the agency.
“There are a small number of unscrupulous actors who have seized on the clinical promise of regenerative medicine, while exploiting the uncertainty, in order to make deceptive, and sometimes corrupt assurances to patients based on unproven and, in some cases, dangerously dubious products,” FDA Commissioner Scott Gottlieb said in a statement Monday. The FDA has taken action against clinics in California and Florida. The agency sent a warning letter to the US Stem Cell Clinic of Sunrise, Fla., and its chief scientific officer, Kristin Comella, for “marketing stem cell products without FDA approval and significant deviations from current good manufacturing practice requirements.”
The clinic is one of many around the country that claim to use stem cells derived from a person’s own fat to treat a variety of conditions, including Parkinson’s disease, amyotrophic lateral sclerosis (ALS), and lung and heart diseases, the FDA says. The Florida clinic had been previously linked to several cases of blindness caused by attempts to use fat stem cells to treat macular degeneration. Stem-cell researchers praised the FDA’s actions.
“This is spectacular,” says George Daley, dean of the Harvard Medical School and a leading stem-cell researcher. “This is the right thing to do.”
Daley praised the FDA’s promise to provide clear guidance soon for vetting legitimate stem-cell therapies while cracking down on “snake-oil salesmen” marketing unproven treatments.
Stem-cell research is “a major revolution in medicine. It’s bound to ultimately deliver cures,” Daley says. “But it’s so early in the field,” he adds. “Unfortunately, there are unscrupulous practitioners and clinics that are marketing therapies to patients, often at great expense, that haven’t been proven to work and may be unsafe. “Others agreed “I see this is a major, positive step by the FDA,” says Paul Knoepfler, a professor of cell biology at the University of of California, Davis, who has documented the proliferation of stem-cell clinics. “I’m hoping that this signals a historic shift by the FDA to tackle the big problem of stem-cell clinics selling unapproved and sometimes dangerous stem cell “treatments” that may not be real treatments,” Knoepfler says.
“Don’t stop now”. Say I. This Blog has been asking for FDA intervention in those settings where Amniotic Fluid is being marketed as a source of stem cell regeneration for over a year. There is only one way to be safe and not sorry:
You may access my web site Ilcellulartherapy.com and watch my webinar Or call for an appointment — 312-475-1893
Tags: arthritis, Benefits and Risk, bone marrow, Bone Marrow Concentrate, Clinical Studies, Concentrated Stem Cell Plasma, Growth Factors, Orthopedics, Osteoarthritis, Pain Management, Regenerative, stem cell treatment, stem cells, treatment

Jul 20, 2017
We now are approaching five-year outcomes regarding the use of Bone Marrow Concentrate for Osteoarthritis of the hip, knee, shoulder and ankle. Bone Marrow contains Adult Mesenchymal Stem (MSC) cells and Growth Factors. In the beginning, the entire informed consent process focused on the MSC in bone marrow as the agent responsible for diminishing pain, improving motion, stopping, at times reversing the progression of osteoarthritis, and potentially regenerating the joint itself. Now we know that equally important to the MSC are the growth factors produced and stored in the bone marrow. Some of the key proteins (Growth factors) include Interleukin-1 Receptor Antagonist Protein (IRAP), Alpha-2-Macroglobulin (A2M), fibrinogen, PDGF, VEGF, and TGF-B to name a few.
The reason we directed our clinical initiatives to Bone Marrow Concentrate is that while Amniotic Fluid contains Hyaluronic Acid, once harvested, sterilized and fast thawed for clinical application, there are no living stem cells left, so Amniotic Fluid Concentrate has no regenerative potential. When it comes to Adipose Derived Stem Cells, in order to liberate the stem cell from the adipocyte, an enzyme, collagenase must be employed. The latter is not approved by the FDA. Additionally, there is no evidence of Growth Factor content in adipose derived tissue.
While I have blogged about the superiority of Bone Marrow Concentrate over all other non-surgical approaches for arthritis, the introduction of the intraosseous adjunct, subchondroplasty, is resulting in even superior outcomes when compared to those who were treated prior to this contemporary version of Cellular Orthopedics. It has been nine months basically since I started injecting Bone Marrow Concentrate into the marrow adjacent to the joint in addition to the intraarticular approach. We already are seeing a better outcome in those who availed themselves of the Intraosseous adjunct. Up until eight weeks ago, my ability to offer contemporary and improved treatment options was limited by preexisting contractual obligations; but now unrestricted, I have expanded my scope of offerings including elevation of subchondroplasty from a clinical trial status to usual and customary adjunct standard of practice option. As well, I now offer an increased opportunity for participation in other clinical trials for the arthritic joint when a patient meets obligatory inclusion criteria determined by the trial sponsor.
If you want to postpone, perhaps avoid a major surgical replacement for an arthritic joint, call for a consultation 847 390 7666
You may visit my web site at IlCellulartherapy.com where you may watch my webinar.
Tags: arthritis, Benefits and Risk, bone marrow, Bone Marrow Concentrate, Clinical Studies, Clinical Trial. Mitchell B. Sheinkop, Interventional Orthopedics, Microfracture surgery, Orthopedics, Osteoarthritis, Pain Management, stem cells, treatment