Jun 14, 2018
Over five years ago, I exchanged a scalpel for a needle and thus entered a developing discipline of cellular orthopedics. My goal was to assist patients with joint afflictions and orthopedic conditions delay, perhaps avoid a surgical procedure by capturing their body’s restorative or regenerative potential and applying evidence-based techniques.
To meet these goals, I introduced the same integration of clinical care with patient outcomes that I had pioneered over a 37-year Joint Replacement career at a major academic orthopedic center in Chicago where I retired as director of the Joint replacement Program. A data base was established and the outcomes of every patient who has undergone a Cellular Orthopedic procedure has been entered into that Data Base regulated by IRB over-site.
Now I am ready to begin sharing the outcomes we have gathered with statistically documented evidence concerning who is a candidate for Cellular Orthopedics, what is the best customized approach for a particular regenerative or restorative procedure and when to advise a patient that surgery might be a better option.
This past weekend, I had a poster exhibit on display at the TOBI meeting in Las Vegas in which I reported preliminary outcomes of a combined Intraarticular and Intraosseous (subchondroplasty) Bone Marrow Concentrate intervention for grades 2 and 3 Osteoarthritis at the knee. I am now working on four presentations as an invited guest speaker at the October meeting of Med Rebels, a well-attended regenerative medicine conference for continuing education credits concerning patient outcomes for different aspects of Cellular Orthopedic recorded in my data base.
What we have learned in these past five years plus is that everyone doesn’t respond to regenerative medicine interventions. You may best gain in-site as to why by reading a blog that I wrote exploring reasons for lack of successes: When Bone Marrow Concentrate Intervention Fails. On the other hand, in part due to the evidence I have gained as well as continuing technological advances, I have a better idea as to who is a candidate for regenerative medicine.
To learn if you are a candidate, schedule a consultation at (312) 475-1893. You may access my web site where you will find my webinar www.Ilcellulartherapy.com.
Tags: arthritis, artificial joint, blood plasma, bone marrow, bone marrow lesion, cellular orthopedics, joint pain, joint replacement, knee pain, Med Rebels, Orthopedic Surgeon, Orthopedics, Osteoarthritis, platelet, stem cells, surgery, TOBI
Feb 16, 2018
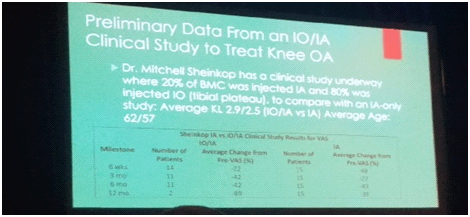
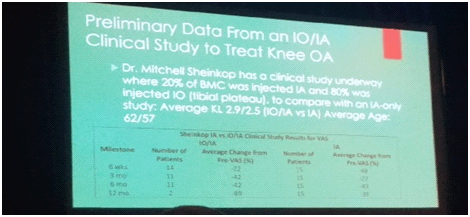
I am sitting at my computer this morning writing the weekly Blog posting and not attending the IOF meeting taking place today in Broomfield, Colorado; yet I am reporting about the meeting. Instead of attending, I am preparing for a week-long ski adventure with my family next week in Vail, Colorado while trying to catch up in my practice. How is it than possible that I know what is taking place at the meeting? Listed below are five of the 10 ongoing or completed cellular orthopedic clinical trials in which I am a principal investigator or co-researcher. The preliminary and final data resulting from these clinical research initiatives is the outcomes foundation for what is being presented at the IOF podium today and tomorrow.
1) Stem Cell Counts and the Outcome of Bone Marrow Concentrate intra-articular and intra-osseous (subchondroplasty) interventions at the knee for grades 2 and 3 OA. (supported in part by Celling). Ongoing
2) Outcomes of Bone Marrow Concentrate (stem cell, platelet and growth factor) Intervention at the Knee for Grades 2 and 3 OA in 50 patients at 2 to 4 years. (supported in part by Regenexx)
3) Outcomes of Intra-articular Bone Marrow Concentrate versus those of combined Intraarticular and Intraosseous interventions for grades 2 and 3 OA at the knee at one year. (self-funded). Ongoing
4) How does the PRP and Mononucleated cell count affect the outcome of a BMC intervention for grades 2 and 3 Knee OA? (a joint project with Greyledge) Ongoing
5) Safety and Efficacy of Percutaneous Injection of Micro-Fractured Adipose Tissue for grade 4 Osteoarthritic Knees, minimum follow-up of 18 months in 30 patients (supported in part by Lipogems)
I had to prioritize; and since most of the arthritis data being presented is all or in part mine, I already know the subject matter. By staying home, I also found the opportunity to browse “stem cell” websites as suggested by ads in today’s newspapers or introduced by email blasts this week. Wow, a patient acting more like a consumer is really at risk for succumbing to Regenerative Medicine “false news”.
If you want to learn more about the difference between the stem cell purveyors and a legitimate, FDA compliant, evidence based, cellular orthopedics initiative, call to schedule a consultation or to get a second opinion.
You may schedule a visit at (312) 475-1893
You may access my website and watch a webinar at www.ilcellulartherapy.com
Tags: arthritis, bone marrow, Celling, cellular orthopedics, Growth Factors, Hip pain, International Orthopedics Foundation, joint pain, knee arthritis, knee intervention, knee pain, lipogems, Micro-Fractured Adipose, Osteoarthritis, PRP, regenerative medicine, Regenexx, stem cells, Subchondroplasty
Dec 20, 2017
Since we practice in an emerging discipline of Regenerative Medicine, how is regeneration determined? Cartilage repair should be evaluated with use of a scoring system that considers the volume of the defect that becomes filled with repair tissue, the integration of repair tissue with adjacent cartilage, and the macroscopic appearance and biomechanical properties of the repair site. The macroscopic assessment is particularly important in evaluating cartilage repair because it provides information about the quality of the full repair site compared to the incidental histological assessment which only evaluates a biopsy of the repair site.
If the aforementioned answer to my introductory question may seem scientifically oriented, that is purposeful on my part; because only those able to explain Regenerative Medicine on a clinical, technical and scientific basis should be caring for your arthritic joint.
While an arthroscopic evaluation provides the best opportunity for a determination of joint regeneration 18 months or greater following a Bone Marrow or Platelet Rich Plasma or other cellular orthopedic intervention for arthritis, an invasive surgical evaluation is not realistic. For a quantitative MRI to assist in the assessment requires availability of a specialized imaging center and there are just too many variables to allow for dependable quantitation; expense is prohibitive. The most dependable and reproduceable means of measuring the arthritic or injured joint response to a cellular orthopedic intervention is a history and physical examination, the latter completed with a tape measure and goniometer as well as an activity assessment. By comparing a baseline measurement prior to an intervention and at serial intervals following the procedure, one may determine if regeneration is indeed taking place and thus establish clinical practice guidelines and determine Evidence Based Quality and Value.
Now for the real question, does cartilage regeneration need to take place on a macroscopic level for cellular orthopedics to succeed? New therapies such as bone marrow derived stem cells, growth factors and cytokines; platelet-rich plasma (PRP); and IRAP (interleukin-1 receptor antagonist protein) first and foremost address the bio-immune basis of degenerative arthritis. By controlling the pain and eliminating inflammation; stopping the progression (at least slowing) of Osteoarthritis; reversing scarring, thus improving motion and function; and lastly, possibly regenerating cartilage for those in whom regeneration is possible. From the editors of the Encyclopedia Britannica: “Interleukin (IL), any of a group of naturally occurring proteins that mediate communication between cells. Interleukins regulate cell growth, differentiation, and motility. They are particularly important in stimulating immune responses, such as inflammation.”
Should our future blogs and discussions address not cartilage regeneration but rather reversing the proinflammatory cytokine production from the synovial lining of the inflamed knee? One such possible pharmacological treatment of OA is anticytokine therapy. Interleukin-1 (IL-1), as a main inflammatory and catabolic cytokine in the pathophysiology of OA, represents one of the possible treatment targets. Koby Bryant was one of the first highly visible professional athletes who travelled to Germany over eight years ago for Interleukin-1 Receptor Antagonist Protein intervention for an arthritic knee. Many, have followed including golfer Fred Couples for his problematic back.
If this Blog has introduced new considerations and questions, then let me clarify. Call 312 475 1893 to schedule an appointment. You may watch my webinar at www.Ilcellulartherapy.com
Tags: arthritis, bone marrow, Hip Replacement, Interleukin, Interleukin-1 Receptor Antagonist, IRAP, Knee Pain Relief, Osteoarthritis, stem cell treatment, stem cells, Subchondroplasty
Dec 14, 2017
After my last blog was posted, a patient sent me a brochure she had received while attending a Regenerative Medicine Seminar focusing on how “stem cell therapy could change your life”. Within the brochure was a full page dedicated to how amniotic fluid stem cell therapy could treat ALS, Autoimmune Disease, Avascular Necrosis, Cartilage Damage, Rheumatoid Arthritis, Traumatic Brain Injury, to name just a few of the 30 listed conditions. The marketing hype went on to indicate “_________ is building the largest network of FDA compliant stem cell centers in the US.”
Last week I emphasized that in order to FDA compliant, Regenerative Medicine must follow several regulatory requirements:
- Minimal Manipulation of the cells or tissue bearing the cells
- Autologous source and homologous application
Minimal manipulation of cells means that they can not be cultured nor can tissues be treated with enzymes to release the stem cells. One such example is a prohibition on fat being subjected to the enzyme collagenase. In simple terms, it is contrary to FDA regulations to perform a liposuction, treat the recovered fat with an enzyme, and inject the cells into a joint or other skeletomuscular structure. As of this writing, I am still seeking clarification on using a mechanical means to emulsify the fat and use the end product in the musculoskeletal system.
Autologous is defined by Merriam-Webster as “involving one individual as both donor and recipient”. It then follows that it is contrary to FDA regulations to use the stem cells in amniotic fluid when recovered by amniocentesis in the musculoskeletal system of a different individual. Add to the latter, the fact that there are no living stem cells in amniotic fluid once sterilized, frozen or lyophilized for preservation and fast thawed for intervention.
Next, I will address homologous as “having the same relation, relative position, or structure” according to the Oxford dictionary. From the FDA oversite standpoint, you can’t put stem cells from amniotic fluid into a joint nor can you introduce fat into a joint. For those patients with arthritis and related orthopedic conditions, beware of the scammers, charlatans and camp followers. As well, for those with degenerative diseases other than orthopedic, be forewarned. There are scoundrels out there very willing to fleece you and take advantage of desperation. For those looking to address non-orthopedic degenerative conditions such as ALS, Autoimmune Disease, Congestive Heart Failure, Multiple Sclerosis, etc., clinical trials are taking place at major medical centers. You may learn about the various trials at NIH.Gov. The FDA warned the non-compliant clinics that they have three years so cheaters will continue to cheat.
From the skeletomuscular and arthritic standpoint, there are clinical specialists available to address your arthritic and other orthopedic problems using FDA compliant Platelet and Bone Marrow derived options just as credentialed as all the other specialties in medicine and surgery. As an orthopedic surgeon, I for one have the scientific outcomes data to support my cellular orthopedic initiatives. To learn more about evidence based cellular orthopedics call 312 475 1893 to schedule a consultation.
Tags: arthritis, bone marrow, Clinical Trial. Mitchell B. Sheinkop, Interventional Orthopedics, Mesenchymal Stem Cell, regenerative medicine, stem cells
Dec 6, 2017
On November 16, 2017, The FDA posted definitive guidelines concerning what meets minimal manipulation rules and regulations and what is accepted under the practice of medicine guidelines in the specialty of Regenerative Medicine. The FDA further restated the requirement that regenerative medicine be governed by homologous use. As I interpret the guidelines there are winners and losers:
Winners
Physicians who use compliant regenerative therapies:
- Amniotic fluid without stem cells
- Blood-derived preparations (e.g., PRP, PPP)
- Bone marrow aspirate
Losers
Physicians who use non-compliant regenerative therapies:
- Adipose tissue-derived materials obtained by enzymatic digestion
- Amniotic fluid with cells Cord blood derived materials (non-autologous treatments)
- Stem Cell Clinics that advertise about using amniotic fluid as a source of stem cells and regenerative therapy along with those clinics that treat everything from alopecia to ALS to arthritis
You might ask how is that different from the current situation? First of all, the FDA Commissioner has stated in press releases that the FDA is going to go after bad actors. The Cures Act provided for increased funding to the FDA, which we suspect the Commissioner will use in part to go after the bad actors. Also, the FDA wrote in their Guidance on Minimal Manipulation and Homologous Use that “healthcare providers” need to pay attention. We have never seen them explicitly refer to the doctors and clinics providing regenerative medicine. Finally, the FDA indicated that there would be a transition period (3 years) during which manufacturers would need to enter the RMAT program to get their non-compliant products properly approved; or else. And the reason that there could be teeth in the “or else” is that the FDA will get lots of fees from all of the non-compliant products entering the RMAT program.
Last of all, what the FDA did not address as part of consumer protection; but what I incorporate in my daily practice is evidence based intervention.
Now that you are better informed and have an idea as to the laws governing our regenerative medicine marketplace, stay away from the Charlatans and Camp Followers. Then take the next step and ask your physician for the Outcomes Evidence on which a regenerative intervention for your arthritic joint is based before undergoing a procedure. To better understand that evidence call for (312) 475 1893 to set up a consultation
You may watch my webinar by accessing my web site www.ilcellulartherapy.com.
* Minimal Manipulation and Homologous Use
Tags: adipose tissue, Bone Marrow Concentrate, Clinical Studies, Clinical Trial. Mitchell B. Sheinkop, FDA, Hip Replacement, Interventional Orthopedics, joint replacement, Mesenchymal Stem Cell, Minimal Manipulation and Homologous Use, Orthopedic Care, Orthopedic Surgeon, Platelet Rich Plasma, PRP, regenerative therapies, stem cells