Feb 28, 2019
My column regarding ACL ruptures appeared last Friday. That afternoon, I received the following inquiry and comment from a reader, regarding the prognosis and possible early preventive interventions for a significant knee injury.
“I am one of relatively few patients who has had the Bone Marrow Concentrate treatment for a fully-torn (not-retracted) ACL tear and to date, I’ve had what I’d consider to be an amazing recovery. I read your latest blog post and just thought I’d let you know that I’m back to very aggressive skiing (including small but non-trivial jumps). However, I did want to ask, if you would be willing to comment, if there are actions or periodic diagnostics, you’d recommend to maximize the chances that I’m still happy skiing 10,20,30 years after the injury? I understand you probably can’t comment but nevertheless wanted to let you know I was also a real-life person who had a significant knee trauma with multiple surgical consults all agreeing it was fully torn and required surgery (to return to high-level skiing) and now have a fairly normal looking ACL in MRI (per independent radiologist) and am back to 100% with activities that require a lot of knee stability. I did do two rounds of same-day BMA reinjections and a bunch of platelet injections but no surgery.”
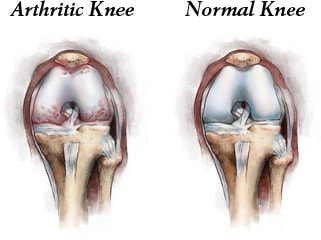
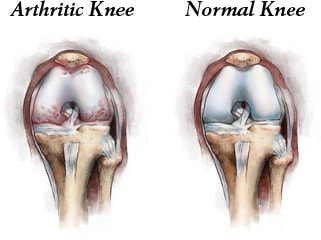
The answer is an orthopedic assessment at three-year intervals to look for markers of post traumatic osteoarthritis such as loss of terminal extension and asymmetrical flexion. The MRI is helpful in detecting moderate arthritic changes but the latest development, the needle scope, allows an orthopedic surgeon to directly examine the meniscus and cartilage in an office setting. The concern is post traumatic arthritis, cartilage defects that will progress, and meniscal damage not always seen on the MRI. Here are some thoughts on early intervention with Cellular Orthopedic and Regenerative Medicine options.
A recent Study Compared the Efficiency of Needle Arthroscopy Versus MRI for Meniscal Tears and Cartilage damage. Needle arthroscopy (NA) may be a less costly and more accurate option for diagnosis and treatment of meniscal tears and early onset post traumatic arthritis than MRI, according to a study published in the February issue of Arthroscopy. Researchers collected data on costs for care and accuracy, including procedures for both false-positive and false-negative findings well as private payer reimbursement rates. They compared outcomes using the global knee injury and osteoarthritis outcome score (KOOS). Patients were followed and evaluated over a two-year period.
There are several restorative options now available when conservative therapies for the treatment of knee degenerative processes, such as non-pharmacological interventions, systemic drug treatment, and intra-articular therapies offer only short-term benefits or fail. Before resorting to surgery; be aware that encouraging preliminary results have been reported using mesenchymal stem cells (MSCs), either alone or in association with surgery. My clinical published research documents success with using your Bone Marrow Concentrate for joint restoration and combating progression of posttraumatic arthritis. Additionally, I have published an article concerning another source for joint restoration, micro-fractured adipose tissue. The latter has created a huge interest in the context of cartilage regeneration due to its wide availability, ease to harvest and richness in mesenchymal cell elements within the so called stromal vascular fraction. Moreover, MSCs from adipose tissue are characterized by marked anti-inflammatory and regenerative properties, which make them an excellent tool for regenerative medicine purposes.
Tags: ACL tear, Adult Mesenchymal Stem Cells, arthritis, Arthroscopy, biologics, bone marrow, cartilage damage, cellular orthopedics, hip pain orthopedic surgeon, joint pain, joint restoration, knee pain, KOOS, meniscal tears, MSC, orthobiologic, Osteoarthritis, PRP, sports medicine, therapy, treatment
Oct 18, 2018
We are speaking of stem cell therapy integrated with clinical research, and the resultant evidence-based stem cell intervention. Osteoarthritis is becoming more prevalent as I am seeing younger patients with arthritis as a consequence of sporting injuries such as ACL tears. The baby boomer population is experiencing accelerated onset of arthritis; their joints are prematurely aging in large numbers. At the same time, the master population is aging and living longer. As a result, I continually research biologic interventions to best address the ever-increasing number of those effected.
Why should a patient choose an orthopedic surgeon to manage their Osteoarthritic related symptoms and functional impairment? Our world is evidence based.
Study Observes Better Outcomes for OA Patients Treated by an Orthopaedic Specialist
In a retrospective study published online in BMC Musculoskeletal Disorders, shoulder osteoarthritis (OA) patients received faster and more invasive treatment when they received a new diagnosis from an orthopaedic specialist (OS) versus a nonorthopaedic physician (NOP). Patients with shoulder OA (n = 572) received care from either an OS (n = 474) or NOP (n = 98) on the date of their index shoulder visit. OS patients received their first treatment significantly quicker than the NOP cohort (16.3 days versus 32.3 days, respectively). The OS group also had higher rates of operative treatment within one year following their initial visit.
Study: Patients Report Similar Improvements for Nonobstructive Meniscal Tear with PT and Early Surgery
Physical therapy (PT) may not be inferior to early operative treatment of arthroscopic partial meniscectomy (APM) for improving knee functionality in patients with nonobstructive meniscal tears, according to a study published online inJAMA. The randomized clinical trial included 321 patients with nonobstructive meniscal tears aged 45 to 70 years who were treated at nine hospitals in the Netherlands between July 17, 2013, and Nov. 4, 2015. Patients were treated with APM (n = 159) or a predefined PT protocol (n = 162) that included 16 exercise therapy sessions over eight weeks. PT sessions focused on coordination and closed kinetic chain strength exercises. At 24-month follow-up, knee functionality in the PT group improved by 20.4 points compared to 26.2 points in the APM group. The difference did not exceed the noninferiority margin.
In order to maximize the benefits, Orthobiologics, that is stem cell therapy must be integrated with clinical research, and the resultant evidence-based stem cell intervention followed long term. In my practice, I am researching biologic interventions to address the ever-increasing number of those effected, not one and done. To learn more or schedule a consultation, Call (312)475-1893. You may visit my web site and read my blogs at www.sheinkopmd.com
Tags: ACL tear, arthritis, Cartilage, cellular orthopedic, joint pain, joint replacement, knee pain, MCL tear, meniscus tear, menisectomy, orthobiologics, orthopedic surgen, Osteoarthritis, Physical Therapy, PRP, regenerative medicine, stem cell

Oct 15, 2016
Background: It is increasingly recognized that biochemical abnormalities of the joint precede radiographic abnormalities of post traumatic osteoarthritis (PTOA) by as much as decades. A growing body of evidence strongly suggests that the progression from anterior cruciate ligament (ACL) injury to PTOA is multifactorial, involving the interplay between biomechanical disturbances and biochemical homeostasis of articular cartilage.
Purpose: A randomized study using an acute ACL injury model were to (1) evaluate the natural progression of inflammatory and chondro-degenerative biomarkers, (2) evaluate the relationship between subjective reports of pain and inflammatory and chondro-degenerative biomarkers, and (3) determine if post injury knee drainage (arthrocentesis) and corticosteroid injection offer the ability to alter this biochemical cascade.
Study Design: Randomized controlled trial.
Methods: A total of 49 patients were randomized to 4 groups: group 1 (corticosteroid at 4 days after ACL injury, placebo injection of saline at 2 weeks), group 2 (placebo at 4 days after ACL injury, corticosteroid at 2 weeks), group 3 (corticosteroid at both time intervals), or a placebo group (saline injections at both time intervals). Patient-reported outcome measures and synovial biomarkers were collected at approximately 4 days, 11 days, and 5 weeks after injury. The change between the time points was assessed for all variables using statistical analysis, and the relationship between changes in outcome scores and biomarkers were assessed by calculating a commonly accepted mathematical analysis. Outcomes and biomarkers were also compared between the 4 groups using another statistical approach.
Results: No adverse events or infections were observed in any study patients. With the exception of matrix metalloproteinase 1 (MMP-1) and tumor necrosis factor–inducible gene 6 (TSG-6), chondro-degenerative markers worsened over the first 5 weeks while all patient-reported outcomes improved during this time, regardless of treatment group. Patient-reported outcomes did not differ between patients receiving corticosteroid injections and the placebo group. However, increases in C-telopeptide of type II collagen (CTX-II), associated with collagen type II breakdown, were significantly greater in the placebo group (1.32 ± 1.10 ng/mL) than in either of the groups that received the corticosteroid injection within the first several days after injury (group 1: 0.23 ± 0.27 ng/mL [P = .01]; group 3: 0.19 ± 0.34 ng/mL [P= .01]).
Conclusion: Post Traumatic Osteoarthritis begins at the time of injury and results early on in dramatic matrix changes in the knee. However, it is encouraging that early intervention with an anti-inflammatory agent was able to affect biomarkers of chondral degeneration. Should early intervention lead to meaningful changes in either the onset or severity of symptomatic PTOA, the current treatment paradigm for patients with ACL injury may have to be restructured to include early aspiration and intra-articular intervention.
This Blog is excerpted from a study appearing in the American Journal of Sports Medicine. My message, should you experience a significant joint injury, don’t wait until arthritic related symptoms appear, the Cellular Orthopedic intervention should take place within weeks; not years.
312-475-4523 to learn more or schedule an appointment
Tags: ACL Injury, ACL tear, arthritis, athletes, Clinical Studies, Clinical Trial. Mitchell B. Sheinkop, corticosteriod injection, Interventional Orthopedics, Knee, knee injury, Microfracture surgery, Orthopedic Care, Orthopedic Surgeon