Feb 4, 2019
On Monday, the annual migration for attempts at the physical Restoration and Regeneration of the NFL players injured bodies began. While in the past, the losers would chant “wait ‘til next year”; very soon, the NFL winners and losers alike will take flight to Orthopedic Surgeons around the USA and world, on occasion, some will even find their way to my office, seeking both operative and non-operative repair of the injuries incurred over the last eight months. What I will offer is Regenerative and Restorative initiatives using either the patient’s bone marrow, circulating blood or body fat. While I use a needle and not a knife in my practice, at times it takes arthroscopy and open surgical procedures to assist the athlete in returning to play or extending a career. The fall NFL 2019 schedule is already on line; there is a sense of urgency. These attempts at restoring and regenerating anatomic and physical well-being are not limited to the professional football player. To the best of my recollection, it was Tiger Woods in 2008, who brought regenerative medicine to the attention of the American public. When in 2011, Kobe Bryant traveled to Dusseldorf, Germany for a highly publicized orthobiologic treatment of his arthritic knee, returning to play for another six seasons, he was soon after followed by the professional golfer Fred Couples, baseball player Alex Rodriguez, and NFL star Payton Manning. All returned to their respective sport and extended playing careers; many more have followed. Now Cellular Orthopedics, Regenerative Medicine and Joint Restoration are available around our country as well as at my office for professional, college, high school, amateur athletes and fitness enthusiasts of any age.
Orthobiologics and Cellular Orthopedics are a dynamic approach to body injury and arthritis using the individual’s own (autologous) platelets, molecules and proteins circulating in the blood (Cytokines and Growth factors), adipose tissue, or bone marrow to effect healing and eliminate pain. At this time, it is FDA Compliant to use such in the care and treatment of injury and arthritis as long as that which is to be used has been harvested from the patient herself or himself, not cultured or expanded, and not treated with additional agents. The successes are no longer merely anecdotal; there is an ever-increasing body of scientific evidence to validate the emerging discipline of Cellular Orthopedics. For instance, in my office, I integrate patient care with documenting outcomes and that has led to several recent scientific publications contributing to an evidence-based orthobiologics practice. You may find those publications and more at my web site www.sheinkopmd.com. To schedule a consultation call (312) 475-1893.
There is a way of still being an athlete and significantly reducing your risk of injury, take up esports. Marquette University is adding varsity esports, a competitive video gaming team in the fall of 2019. The team will have tryouts, coaches and regular practices just like any intercollegiate sport
Tags: arthritis, athletes, autologous, avascular necrosis, bone marrow, cellular orthopedics, cytokines, esports, Growth Factors, injury, joint pain, joint replacement, joint restoration, knee pain, meniscus tear, MSC, OA, orthobiologic, Orthopedic Surgeon, Osteoarthritis, Pain Management, pain reduction, patyon manning, platelets, PRP, sports injury, sports medicine, stem cells, superbowl, surgery, tiger woods, torn labrum
Nov 15, 2018
Mesenchymal Stem Cells, or MSCs, are multipotent stromal cells that can differentiate into a variety of cell types or affect other cells by releasing the proteins categorized as Cytokines and Exosomes. Cytokines are small proteins that are important in cell signaling. The process is quite complex but this introduction allows me to help you better understand the Regenerative Medicine world.
The patient who called this morning indicated that she had not experienced any benefit form an orthobiologic intervention she had several weeks ago; yet on Friday, several patients reported satisfaction and our outcomes surveillance documented significant functional improvement as well. Why the variability in response? Perhaps it might or could be explained by the genetic makeup of the individual’s cartilage or the nature of the biologic intervention. In the current regenerative marketplace, I note advertisements for Amniotic Fluid, Cord Blood, Wharton’s Jelly, Exosomes, Adipose derived and bone marrow derived interventions.
The long-term durability of our cellular orthopedic treatment has been documented in patients for at least five years. The observation of this response is significant, as steroids and viscosupplementation have typically shown to be effective in relieving pain respectively for up to 6 weeks and 6 months. Our earlier research has documented a six-month average response to amniotic fluid and an average 18-month improvement to mechanically processed adipose tissue. Our current biologic interventions contain high concentrations of anti-inflammatory cytokines and anabolic growth factors in addition to Mesenchymal Stem Cells, all modifying the course of disease progression. The short-term pain relief observed is due to the anti-inflammatory effects of the biologics used in the interventions. The long-term pain relief is attributed to potential disease-modifying properties by improving joint homeostasis and cartilage quality. We believe our biologic interventions to be disease-modifying.
What is next? While most readers of this Blog are familiar with the regenerative alternatives, Exosomes are new and there is little if any clinical data available to allow me to opine about clinical usage including safety and efficacy at this time. They are cell-derived vesicles (a small membrane-bound sack that stores and transports substances though out the cell or outside the cell) present in bodily fluids as well as in extracellular matrix. Evidence is accumulating that they play a key role in signaling between cells and may function as a potent anti-inflammatory and disease modifier depending on the environment from which the Exosome is recovered. While the use of non-autologous stem cells is not FDA compliant, to the best of my knowledge, Exosomes produced by Mesenchymal Stem Cells are not restricted and are now being made available for clinical use in arthritis. Stay tuned as we continue to document successes, safety and efficacy in the world of Orthobiologics. To learn more, schedule a consultation by calling (312) 475-1893.
Tags: arthritis, biologics, cytokines, Exosomes, Growth Factor Concentrate, Growth Factors, Mesenchymal Stem Cell, MSC, OA, viscosupplementation

Aug 30, 2018
Evidence for the efficacy of Platelet Rich Plasma, a blood-derived formulation, and bone marrow derived biologics in osteoarthritis continues to grow in the orthopedic community. On the other hand, as I continually monitor the current landscape of indiscriminate and sometimes inappropriate marketing and use of biologics by the non-orthopedic opportunists, I doubt if the charlatans and camp followers have an overview of what is known about these agents. The increased presence of clinics Is driven by the popularity of PRP and its biologic cousins:
- consumer demand
- aggressive marketing
- a low regulatory bar for many of these regenerative medicine clinics
- the autologous nature that makes many approaches largely safe
- positive data from centers such as ours demonstrating functional and symptom modification
PRP works by activating cellular pathways; more than 3,000 genes are related to these and other pathways, suggesting that PRP probably acts by inducing a transitory inflammatory event, which then triggers tissue regeneration. Bone Marrow Concentrate, does more and addresses the subchondral bone when appropriately injected as well as initiate joint preservation and possible regeneration.
Taking aim
I use a hemoanalyzer to characterize a dose of PRP or Bone Marrow Concentrate allowing me to quantify the composition and biologic activity of these agents. Soon, I will begin pretreatment assessment of the synovial fluid of the arthritic joint so as to best determine who is the optimal candidate for a particular procedure
What do we know?
- Knee osteoarthritis: white blood cell-poor PRP has a positive effect on symptoms, not structure; while Bone marrow Concentrate affects symptoms and structure. I identify what I am putting into the patient. My goal is to have reliable predictors of outcome; that is, do the composition and biologic activity of the material implanted in the patient predict the clinical/imaging outcomes? My PRP contains a high concentration of anti-inflammatory cytokines and anabolic growth factors whereas my use of Bone Marrow Concentrate inside the bone adjacent to the joint in addition to the joint itself is improving the outcomes of the patients I treat.
- To learn more, call my office to schedule an appointment at (312) 475-1893
- You may view my Web site at WWW.Sheinkopmd.com
Tags: anit-inflammatory, biologics, bone marrow, cellular orthopedic, cellular therapy, cytokines, knee osteoarthritis, Orthopedic Surgeon, PRP, regenerative medicine, stem cell
Jan 5, 2018
If you read my blog posting last week, you would have learned that I personally underwent a cellular orthopedic intervention to both of my knees on Wednesday, 12/27. The symptoms attributable to my own osteoarthritis had progressed to a degree that I was becoming limited in my recreational profile. While there indeed was a response to anti-inflammatory medications, every time I am reminded of the potential complications of NSAIDS, I become medication adverse. This led to the injection into both of my knees of an Autologous Protein Concentrate (APC) with the hope of treating my pain and slowing the progression of cartilage degradation and destruction of my knees.
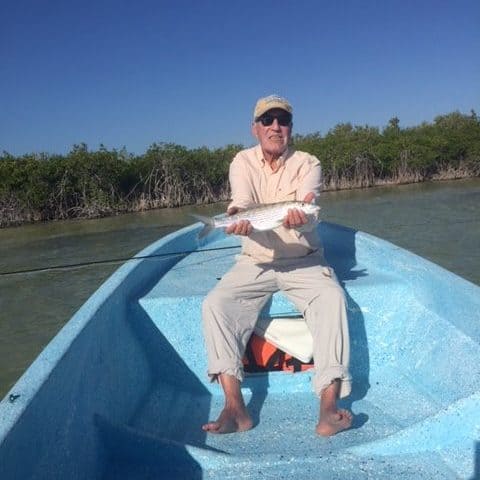
The process used was a cell-concentration system which concentrated my own anti-inflammatory cytokines and anabolic growth factors. Pioneered in Europe, an ever-increasing number of professional athletes have been prolonging their careers by accessing this treatment. I have waited over five years for the Autologous Protein Concentrate methodology to become available in the United States; three weeks ago, I was granted access. To date, my pain secondary to knee osteoarthritis is not only reduced but gone; I can only hope it stays that way. My function is significantly improved as evidenced by an ability to have pursued my fly fishing passion chasing bone fish with my wife, daughter-in-law and son for three days in Ascension Bay, Mexico, over the New Year weekend. For those unfamiliar, bone fishing requires a continued down and up to a platform on the front of a three-man boat with prolonged standing while balancing. At times, I climbed out of the boat and waded through the flats for 30 to 45-minute intervals until it was time to change locations. Since returning home on January 1, I have been able to return to my fitness profile without restriction previously afforded by my Osteoarthritis generated symptoms and limitations.
As in any and all treatments, a patient must be given informed consent and be warned both of the benefits and risks; so, I will let you in on an adverse event in my early outcome. Owing to the increased activity attributable to the diminution of my pain and increased functional capacity resulting from my initial response to the Autologous Protein Concentrate intervention, instead of climbing down from the fly fishing platform in the front of our boat when it was time to trade places with my wife, I jumped down. In so doing, I kicked the rod holding rack and fractured the fifth toe on my left foot, the pinky toe. Though a bit of a nuisance, it is not too great a price to pay for the relief and improved function of my knees.
To learn more, call my office and schedule an appointment; as I haven’t yet updated my web site with an explanation of the Autologous Protein Concentrate intra-articular injection for treatment of knee osteoarthritis (312) 475-1893.
Tags: anti-inflammatory, arthritis, Autologous Protein Concentrate, cytokines, Growth Factors, Hip Replacement, horse, injection, Interventional Orthopedics, joint replacement, Knee Pain Relief, Osteoarthritis, Pain Management, regenerative medicine, rheumatoid arthritis, treatment, treatment of equine lameness